 Refers to extrinsic allergic alveolitis.
Refers to extrinsic allergic alveolitis.
A form of interstitial lung disease.
Non-IgE mediated inflammatory interstitial pulmonary disease caused by inhalation of small organic antigens.
prevalence rates in the US range from 1.67 to 2.71 per 100,000, with prevalence increasing with age.
More than 200 antigens have been identified as causing this process.
Can be an acute, sub acute or chronic process.
Acute disease typically results in shortness of breath, dry cough, fever and malaise four to six hours after exposure to the antigen.
Sub acute disease occurs in patients who have recurrent low-level exposure to the antigen.
Chronic disease may occur with persistent or frequent exposure to the antigen and eventually lead to irreversible pulmonary fibrosis.
Primarily occurs in adults related to occupations or hobbies.
Uncommon in children.
Less than 5 microm organic airborne inhaled antigens activate lung alveolar macrophagesis in the distal lung and induce a cascade of inflammatory cytokines with type III and type IV hypersensitivity rections.
Generally, the aerosol particles or equal or less than three micro millimeters enabling them to reach the alveolus.
Results in a interstitial inflammatory process with infiltration of lymphocytes, plasma cells, and formation of noncaseating granulomas.
Poorly formed granulomas are present, and they may be associated with multinucleated giant cells near the respiratory or terminal bronchioles.
Well formed granulomas are not common.
The pathological findings is not a vasculitis and is not associated with elevated IgE levels.
Levels of precipitating antibodies to the inciting antigen are commonly elevated in the serum, and these antibodies are usually of the IgG subclass but may be of the IgA or IgM subclass.
The presence precipitating antibodies is not specific for this process as such antibodies may be present in exposed persons without the disease.
Cytokines involved include gamma-interferon, IL-1 and TNF-alpha.
BAL cellularity is markedly increased with a striking lymphocytosis.
The ratio of CD4+ to CD8+ lymphocytes is less than 1% in BAL fluid (Drent M).
Dairy farmers are risk as they work with hay, grains and silage with the exposure of thermophilic actinomycetes.
Avian proteins can cause the process in bird keepers and pigeon breeders, as they are exposed to avian droppings or feathers.
May result in humidifier users from contamination of water and the development of offending microorganisms.
Chemical workers exposed to polyurethane foam, vanishes, and lacquers containing isocyanates may suffer from this process.
May be seen in metal workers, utilizing metalworking fluids in the presence of various bacterial contaminants.
Contaminated wood dust with Bacillus subtilis and mold may be responsible for hypersensitivity pneumonitis.
Occurs almost exclusively in non-smokers, as it is suspected that tobacco may have immunosuppressive effects.
Chest x-rays in acute disease often show reticulonodular infiltrates in the lower lung.
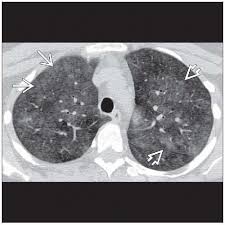
High resolution CT scans of the chest may show ground glass opacities and micronodules.
High resolution CT scans in subacute or chronic disease may show micronodules, fibrosis and attenuation.
Diagnosis requires a complex of historical, radiologic and pathologic findings.
Process develops after exposure to aerolized antigenic stimulus in a susceptible individual.
For most patients, the avoidance of the antigen results in more clinical improvement.
In patients with severe disease antigen avoidance with the use of corticosteroids over a few weeks is recommended treatment (Patel AM).
Complete and immediate avoidance of the offending antigen is required, because continued exposure will result in progressive lung damage.
Antibiotics and immunosuppressive agents are not indicated therapies.
Patients with subacute and chronic disease usually have symptomatic improvement, and some improvement in pulmonary function testing, but complete normalization of pulmonary function is rare.
Because it is a immune-mediated disease repeat antigen exposure can result in recurrence of symptoms.
