
 Refers to a disorder of cerebrospinal fluid physiology with abnormal expansion of the cerebral ventricles, typically associated with increased intracranial pressure.
Refers to a disorder of cerebrospinal fluid physiology with abnormal expansion of the cerebral ventricles, typically associated with increased intracranial pressure.
Hydrocephalus refers to a condition in which an accumulation of cerebrospinal fluid (CSF) occurs within the brain.
It typically causes increased pressure inside the skull.
The cause of hydrocephalus is not known with certainty, but may be caused by impaired CSF flow, reabsorption, or excessive CSF production.
Most common disease treated by a pediatric neurosurgeons.
Accounts for roughly $2 billion and health expenses annually in the US.
Older people may have headaches, double vision, poor balance, urinary incontinence, personality changes, or mental impairment.
In babies, it may be seen as a rapid increase in head size.
Symptoms may include vomiting, sleepiness, seizures, and downward pointing of the eyes on babies.
Symptoms
Babies: rapid head growth, vomiting, sleepiness, seizures.
Older people: Headaches, double vision, poor balance, urinary incontinence, personality changes, mental impairment
Incidence greater in developing countries.
The most common cause in high income countries are post hemorrhagic hydrocephalus of prematurity, congenital aqueduct stenosis, myelomeningocele, and brain tumors.
Causes of hydrocephalus:
Neural tube defects, meningitis, brain tumors, traumatic brain injury, brain bleed during birth, intraventricular hemorrhage.
Frequency from 1 per 256 live births to 1 per 9,000, depending on access to prenatal health care, prenatal tests, and abortion.
Hydrocephalus can occur due to birth defects or be acquired later in life.
H is associated birth defects including neural tube defects and those that result in aqueductal stenosis.
About one to two per 1,000 newborns have hydrocephalus.
Rates in the developing world may be higher.
Other causes: meningitis, brain tumors, traumatic brain injury, intraventricular hemorrhage, and subarachnoid hemorrhage.
The four types of hydrocephalus are communicating, noncommunicating, ex vacuo, and normal pressure.
CSF is secreted by the choroid plexus epithelium in the cerebral ventricles and flows into the subarachnoid spaces, and enters the cerebral venous system did the arachnoid granulations.
Every day, the body makes roughly 600–700 ml of CSF, and about the same amount is reabsorbed into the bloodstream.
Hydrocephalus is due to an imbalance between the amount of fluid produced and its absorption rate.
It is proposed that obstruction to the CSF anywhere from its origin to most distal point of absorption may result in hydrocephalus.
In a few cases hypersecretion of CSF may be the cause.
Obstruction of CSF within the ventricles can be classified as obstructive or non-communicating hydrocephalus.
Obstruction of CSF flow or it’s absorption in the subarachnoid space is known as communicating hydrocephalus.
Ventricular or subarachnoid space obstruction and raised cerebral venous pressure can lead to hydrocephalus.
Enlarged ventricles put increased pressure on the adjacent cortical tissue and cause myriad effects in the patient, including distortion of the fibers in the corona radiata.
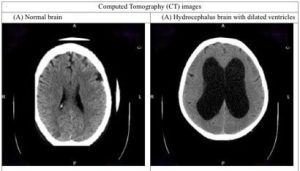
Diagnosis: by physical examination and medical imaging.
H is typically treated by the surgical placement of a shunt system.
A third ventriculostomy is an option in some cases.
Complications from shunts: overdrainage, underdrainage, mechanical failure, infection, or obstruction.
Such complications may require shunt replacement.
Many patients with shunts live normal lives, and without treatment, death or permanent disability may occur.
Normal pressure hydrocephalus is estimated to affect about 5 per 100,000 people, with rates increasing with age.
The clinical presentation of hydrocephalus varies with its chronicity.
Acute dilatation of the ventricular system is more likely to manifest with the nonspecific signs and symptoms of increased intracranial pressure (ICP).
Chronic dilatation, especially in the elderly, may have a more insidious onset presenting, for instance, with Hakim’s triad (gait instability, urinary incontinence, and dementia).
Symptoms of increased ICP may include headaches, vomiting, nausea, papilledema, sleepiness, or coma.
With increased levels of CSF, hearing loss due to CSF creating pressure on the auditory pathways or disrupting the communication of inner ear fluid may occur.
Elevated ICP has been linked to sensorineural hearing loss.
Elevated ICP may result in uncal or tonsillar herniation, with resulting life-threatening brain stem compression.
Hakim’s triad of gait instability, urinary incontinence, and dementia is typical manifestation of the distinct entity normal-pressure hydrocephalus.
Normal-pressure hydrocephalus may be associated with focal neurological deficits, such as abducens nerve palsy and vertical gaze palsy (Parinaud syndrome).
Hydrocephalus symptoms depend on the cause of the blockage, the person’s age, and how much brain tissue has been damaged by the swelling.
Infants with hydrocephalus build up fluid in the central nervous system (CNS), causing the soft spot to bulge and the head to be larger than expected.
Early symptoms in infants with hydrocephalus may include:
Eyes that appear to gaze downward
Irritability
Seizures
Separated sutures
Sleepiness
Vomiting
Symptoms in older children can include:[
Brief, shrill, high-pitched cry
Changes in personality, memory, or the ability to reason or think
Changes in facial appearance and eye spacing
Crossed eyes or uncontrolled eye movements
Difficulty feeding
Excessive sleepiness
Headaches
Irritability, poor temper control
Urinary incontinence
Loss of coordination and trouble walking
Muscle spasticity
Slow growth
Delayed milestones
Failure to thrive
Slow or restricted movement
Vomiting
Thought and behavior may be adversely affected.
Learning disabilities, including short-term memory loss.
Scoring better on verbal IQ than on performance IQ, which is thought to reflect the distribution of nerve damage to the brain.
Hydrocephalus present from birth can cause long-term complications with speech and language, nonverbal learning disorder, difficulty understanding complex and abstract concepts, difficulty retrieving stored information, and spatial/perceptual disorders.
The severity of hydrocephalus differs considerably between individuals, and some are of average or above-average intelligence.
Someone with hydrocephalus may have coordination and visual problems, or clumsiness.
Some patients experience precocious puberty.
About 25% develop epilepsy with hydrocephalus.
Congenital hydrocephalus means the fetus developed hydrocephalus in utero during fetal development.
The most common cause of congenital hydrocephalus is aqueductal stenosis, which occurs when the narrow passage between the third and fourth ventricles in the brain is blocked or too narrow to allow sufficient cerebral spinal fluid to drain.
In such cases fluid accumulates in the upper ventricles, causing hydrocephalus.
Congenital hydrocephalus include: neural-tube defects, arachnoid cysts, Dandy–Walker syndrome, and Arnold–Chiari malformation.
The cranial bones fuse by the end of the third year of life.
For head enlargement to occur, hydrocephalus must occur before then.
Congenital hydrocephalus causes are usually genetic, but can also be acquired and usually occur within the first few months of life, intraventricular matrix hemorrhages in premature infants, infections, type II Arnold-Chiari malformation, aqueduct atresia and stenosis, and Dandy-Walker malformation.
Hydrocephalus has also been seen in cases of congenital syphilis.
In newborns and toddlers with hydrocephalus, the head circumference enlarges rapidly.
Newborns with hydrocephalus exhibit fretfulness, poor feeding, and frequent vomiting, and eventually torpor, and lack of interest in their surroundings.
Subsequently, infants’ upper eyelids become retracted and their eyes are turned downwards, with ssunset eyes due to hydrocephalic pressure on the mesencephalic tegmentum and paralysis of upward gaze.
These infants become weak and the arms may become tremulous.
Papilledema is absent, but vision may be reduced.
The head becomes so enlarged that they eventually may be bedridden.
About 80–90% of fetuses or newborn infants with spina bifida, often associated with meningocele or myelomeningocele develop hydrocephalus.
Hydrocephalus can be acquired as a consequence of CNS infections, meningitis, brain tumors, head trauma, toxoplasmosis, or intracranial hemorrhage, subarachnoid or intraparenchymal, and is usually painful.
Obstruction to CSF flow hinders its free passage through the ventricular system and subarachnoid space: stenosis of the cerebral aqueduct or obstruction of the interventricular foramina secondary to tumors, hemorrhages, infections or congenital malformations and can causes increased ICP.
Hydrocephalus can also be caused by overproduction of CSF by choroid plexus papilloma, or villous hypertrophy.
Hydrocephalus can be classified into communicating and noncommunicating (obstructive), and both forms can be either congenital or acquired.
Communicating hydrocephalus, is also known as nonobstructive hydrocephalus.
Communicating hydrocephalus is caused by impaired CSF reabsorption in the absence of any obstruction of CSF flow between the ventricles and subarachnoid space.
Communicating hydrocephalus may be due to functional impairment of the arachnoidal granulations, or Pacchioni’s granulations, which are located along the superior sagittal sinus, and is the site of CSF reabsorption back into the venous system:
subarachnoid/intraventricular hemorrhage, meningitis, congenital absence of arachnoid villi, scarring and fibrosis of the subarachnoid space following infectious, inflammatory, or hemorrhagic events can also prevent reabsorption of CSF, causing diffuse ventricular dilatation.
Noncommunicating hydrocephalus, or obstructive hydrocephalus, is caused by an obstruction to the flow of CSF.
Foramen of Monro obstruction may lead to dilation of one, or if large enough to both lateral ventricles.
The aqueduct of Sylvius, normally narrow, may be obstructed by a number of genetic or acquired lesions, as atresia, ependymitis, hemorrhage, or tumor can lead to dilation of both lateral ventricles, as well as the third ventricle.
Fourth ventricle obstruction leads to dilatation of the aqueduct, as well as the lateral and third ventricles, as in Chiari malformation.
The foramina of Luschka and foramen of Magendie may be obstructed due to congenital malformation, as with the Dandy-Walker malformation.
Normal pressure hydrocephalus (NPH) is a particular form of chronic communicating hydrocephalus, characterized by enlarged cerebral ventricles, with only intermittently elevated cerebrospinal fluid pressure.
Characteristic triad of symptoms are; dementia, apraxic gait and urinary incontinence.
The diagnosis of NPH can be established only with the help of continuous intraventricular pressure recordings over 24 hours or even longer.
In NPH, more often than not, instant measurements yield normal pressure values.
Altered elasticity of the ventricular walls, as well as increased viscosity of the cerebrospinal fluid, may play a role in the pathogenesis.
Hydrocephalus ex vacuo also refers to an enlargement of cerebral ventricles and subarachnoid spaces, and is usually due to brain atrophy, post-traumatic brain injuries, and even in some psychiatric disorders, such as schizophrenia: As opposed to hydrocephalus, this is a compensatory enlargement of the CSF-spaces in response to brain parenchyma loss, and it is not the result of increased CSF pressure/
Hydrocephalus is usually due to blockage of CSF outflow in the ventricles or in the subarachnoid space over the brain.
Normally CSF continuously circulates through the brain, its ventricles and the spinal cord and is continuously drained away into the circulatory system.
Alternatively, the condition may result from an overproduction of the CSF, from a congenital malformation blocking normal drainage of the fluid, or from complications of head injuries or infections.
The accumulation of fluid eventually may cause neurological symptoms such as convulsions, intellectual disability, and epileptic seizures by brain compression.
Neurologic signs occur sooner in adults, as a fixed skull is no longer able to expand to accommodate the increasing fluid volume within.
Fetuses, infants, and young children with hydrocephalus typically have an abnormally large head, as the pressure of the fluid causes the individual skull bones, which have yet to fuse, to bulge outward.
In infants, a characteristic fixed downward gaze with whites of the eyes showing above the iris is seen with hydrocephalus.
The mechanism of ICP on hearing loss is presumed that the transmission of CSF pressure to and from the perilymphatic space through a patent cochlear aqueduct.
A loss of CSF pressure can induce perilymphatic loss or endolymphatic hydrops resembling the clinical presentation of Ménière’s disease associated hearing loss in the low frequencies.
CSF can accumulate within the ventricles, this condition is called internal hydrocephalus and may result in increased CSF pressure.
Consequently, fluid builds inside the brain, causing pressure that dilates the ventricles and compresses the nervous tissue.
Compression of the nervous tissue usually results in irreversible brain damage.
If the skull bones are not completely ossified when the hydrocephalus occurs, the pressure may also severely enlarge the head.
The cerebral aqueduct may be blocked at the time of birth or may become blocked later in life because of a tumor growing in the brainstem.
TREATMENT:
Treatment is surgical, creating a way for the excess fluid to drain away.
A ventriculostomy, provides relief.
A cerebral shunt involves the placement of a ventricular catheter into the cerebral ventricles to bypass the flow obstruction/malfunctioning arachnoidal granulations and drain the excess fluid into other body cavities, from where it can be resorbed.
Most shunts drain the fluid into the peritoneal cavity
Alternative sites include the right atrium (ventriculoatrial shunt), pleural cavity (ventriculopleural shunt), gallbladder, and the lumbar space of the spine and have the CSF redirected to the peritoneal cavity (lumbar-peritoneal shunt).
An alternative treatment for obstructive hydrocephalus in selected people is the endoscopic third ventriculostomy:
a surgically created opening in the floor of the third ventricle allows the CSF to flow directly to the basal cisterns, shortcutting any obstruction, as in aqueductal stenosis.
For infants, endoscopic third ventriculostomy is sometimes combined with choroid plexus cauterization, which reduces the amount of cerebrospinal fluid produced by the brain.
External hydrocephalus involves enlarged fluid spaces or subarachnoid spaces around the outside of the brain.
External hydrocephalus is generally benign, and resolves spontaneously by two years of age, and therefore usually does not require insertion of a shunt.
Examples of possible complications include shunt malfunction, shunt failure, and shunt infection, along with infection of the shunt tract following surgery.
Shunt failure occurs if it disconnects, becomes clogged or infected, or it is outgrown.
If shunt failure occurs CSF begins to accumulate again and a number of symptoms develop including: headaches, nausea, vomiting, photophobia/light sensitivity, in extreme cases seizures.
The shunt failure rate is also relatively high -40,000 surgeries performed annually to treat hydrocephalus.
Patients not uncommonly have multiple shunt revisions within their lifetimes.
If CSF drains more rapidly than it is produced by the choroid plexus it may cause symptoms of listlessness, headaches, irritability, light sensitivity, sound sensitivity, hearing loss, nausea, vomiting, dizziness, vertigo, migraines, seizures, a change in personality, weakness in the arms or legs, strabismus, and double vision to appear when the person is vertical: Lying down resolves the symptoms.
Decreased post-surgery hearing following placement of a ventriculoperitoneal shunt may occur and is presumed that perilymphatic pressure in the cochlea aqueduct is responsible for the decrease in hearing thresholds.
Preventative antibiotics may decrease the risk of shunt infections.
