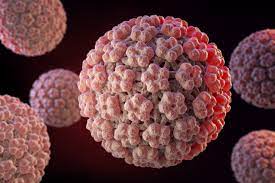
 A virus that can infect the skin and mucosal surface of the oral pharynx, throat, and anogenital area.
A virus that can infect the skin and mucosal surface of the oral pharynx, throat, and anogenital area.The most common sexually transmitted infection in the US.
HPV’s can establish a persistent reservoir of infection, while evading the host immune system, and commonly shedding cells containing viral particles.
The virus infects and takes advantage of a stratified, differentiated epithelium, persisting, and dividing in basal cells, and only produces viral particles in the terminally differentiating outermost layers of the epithelium.
Most of the sexually active population is estimated to be infected with HPV during their lifetimes, and a positive HPV test is considered a marker of sexual activity.
Globally almost 1/3 of men have a genital HPV infection, and about one and five have high risk HPV.
Cancer develops in people with persistence of an HPV infection not controlled by the immune system.
Estimated prevalence of the human papilloma virus in the population range as high as 79%, encompassing those with evident clinical disease and those carrying the virus sub clinically.
HPV is the most common sexually transmitted infections worldwide.
Affects 80% of individuals.
Currently estimated 79 million Americans are carriers of at least 1 type of HPV, and about 14 million become infected each year.
Initial infection usually occurs between the ages of 15 and 24.
Majority of individuals who engage in sexual activity will become infected at some point in their lifetime with HPV.
Most HPV infections are not noticed, and more than 90% of the infections clear to become undetectable within 1 to 2 years.
More than 20 HPV virus are known to infect the genital tract.
HPV type 6 and 11 cause about 90% of genital warts.
The majority of patients with HPV infection will be asymptomatic, and clear the virus in 90% of cases, within 1-2 years.
Types 16, 18, 31, 33, 45, 52, and 58 are considered high risk oncogenotypes and are responsible for an estimated 44,000 US cases of cancer each year.
In the US, the most common HPV attributed to cancers of cervical cancers, approximately 11,100 cases per year, and oropharyngeal cancers, approximately 14,800 cases per year, most of which occur in men.
HPV-16 and HPV-18 are responsible for the development of the majority of carcinomas arising from the cervix, greater than 90%, anus, greater than 90%, vagina/vulva greater than 60%, and penis 50%.
Worldwide an estimated 690,000 cancers are attributable tHPV each year.
Virtually all cervical cancers contain, at least one of 13 carcinogenic HPV genotypes.
Carcinogenic HPV genotypes are linked to the alpha genus.
HPV 16 is the most carcinogenic associated with more than 60% of cervical squamous cancers, and adenocarcinomas and oropharyngeal and other anogenital cancers.
Rates of cervical cancer are highest among Black and Hispanic women, and rates of oral pharyngeal cancer, highest among white men.
HPV infection causes up to 4.5% of all new cancer cases worldwide and represents 29.5% of all infection related cancers.
HPV causes 90% of US cervical cancers and 70% of US oropharyngeal cancers and less commonly anal, vaginal, vulvar, and penile cancer.
10% of patients with HPV infection will develop a chronic process with an increased risk of the development of cancer.
Approximately half of the patients with HPV infection will develop a malignancy by 30 years.
Persistent infection with oncogenic HPV genotypes, primarily 16, and 18, is the cause of virtually all cervical and anal cancers, as well as the majority of oropharyngeal, vaginal, vulvar and penile cancers.
More than 200 genotypes have been identified.
Selectively infects skin and mucous membranes.
Of the over 200 different types of HPV, approximately 40 are known to affect the epithelial tissue of the anogenital area and have different probabilities of causing malignant changes.
12 types are defined as oncogenic, and 8 to 12 types as possibly oncogenic.
HPV 16 has the highest risk of progression to cancer.
Worldwide HPV 16 and HPV 18 are responsible for approximately 70% of cervical cancers.
HPV6 and HPV11 cause almost all cases of anogenital warts and recurrent respiratory papillomatosis.
Broadly categorized into high risk and low risk subtypes on the basis of association with high-grade dysplasia versus condylomata and mostly low-grade dysplasia, respectively.
HPV infection begins with direct skin/mucosal contact and inoculation of immortalized basal lamina cells through micro-abrasions that accompany sexual behavior.
Infected basal cells ascend the epidermis, and HPV stimulates cell proliferation into conylomata or dysplasia, completes its lifecycle, and sheds further visions.
Most individuals clear infection, but others have persistence particularly with type 16 HPV, which may progress from low-grade dysplasia through a high-grade form and become malignant.
Approximately 80% of sexually active women contract HPV during their lifetime.
Rates of infection in young sexually active females range from 19-46%.
Prevalence estimated as high as 40% among sexually active females ages 14-19 years and 49% among those ages 20-24 years (Dunne EF).
Estimated to be the most common sexually transmitted infection in the U.S.
Prevalence highest among young individuals within the first few years after initiating sexual activity.
HPV infection rates highest in younger women and it increases rapidly after the median age of first sexual activity at 16.9 years (Wulf D).
Women who begin to have sexual relations at younger ages and those with more sexual partners are at highest risk for exposure to HPV.
HPV integrates its viral DNA into the human genome, express oncogenes, inactivates tumor suppressor genes, and transforms the site of infection with damaged and unchecked proliferation of cells with oncogenesis.
Estimated to be associated with 25,000 cancers annually in the United States.
HPV infection may lead to an overexpression a viral oncogenes E6 and E7.
Viral oncogene E6 binds cycle cell regulatory proteins p53 leading to its degradation and subsequent uncontrolled tumor cell growth.
E7 has an additive oncogenic function binding to and degrading Rb, a tumor suppressor that blocks exit from the G1 phase of the cell cycle, thus regulating E2F transcription factors.
HPV responsible for up to 90% of anal cancers, 65% vaginal cancers, 50% of a vulvar cancers, 35% of penile cancers, and 45-90% of oropharyngeal cancers.
HPV- 10% of patients who had a high-grade squamous intraepithelial lesion (HGSIL, which includes so-called moderate-to-severe dysplasia, carcinoma in situ [CIS], and cervical intraepithelial neoplasia [CIN] II and III) will have persistent lesions that eventually will progress to invasive cancer without treatment.
Penile, vulvar, vaginal, anal carcinomas, and head and neck cancers have been linked to HPV infection.
Children with anogenital warts
Pregnant women with genital warts can transmit the virus to the newborn.
About 5% of all births in the United States are at risk for neonatal HPV exposure.
Infants can develop laryngeal papillomatosis in the first 5 years of life after neonatal HPV exposure.
Approximately 60% of mothers with infants with laryngeal papillomatosis report having genital warts.
Immunosuppressed patients or more likely to develop persistent HPV infection and subsequent dysplasia and malignancy.
Verrucous carcinoma of the genitalia is a low-grade, locally invasive squamous cell carcinoma that is associated with HPV types 6 and 11
HP the associated cancers in males include some anal, penile, and oropharyngeal cancers are caused primarily by HPV 16.
There are estimated 7000 HPV 16 and 18 associate cancers in males in the United States annually.
HPV positive oropharyngeal tumors are increasing in incidence and exceed such lesions caused by the more traditional risk factors of tobacco and alcohol.
There has been increases in the incidence of oropharyngeal and anal cancers in men with approximately 1% per year increase for oral pharyngeal cancers and 3% /year for anal cancers.
Oral HPV infection is a cause of a subset of oropharyngeal squamous cell carcinoma and is associated sexual behavior in contrast to HPV negative oro- pharyngeal squamous cell cancer which is associated with chronic tobacco and alcohol use.
At least 90% of HP positive oral pharyngeal squamous cell carcinoma is are associated with HPV types 16 and oral infection confers an approximate 50 fold increase in the risk of HPV positive moral pharyngeal squamous cell carcinoma (Gillison ML et al).
Genital infection common process with an estimated 6.2 million new cases per year in the U.S.
HPV transmitted by skin or mucosal contact, almost exclusively through sexual activity.
The rate of genital HPV infections is similar in females and among males.
In any year the probability of acquiring a new genital HPV infection in a male is 0.29-0.39 per 1000 person months, which is similar to the statistics for females.
The proportion of females HPV seropositive is 17.9% versus males at 7.9% indicating that females have a higher titer of antibodies than males.
Males have a lower immune response to natural infection to HPV virus and have a higher prevalence of HPV infections, as compared with the prevalence among females.
Oral and digital infections with genital HPV strains occur but are associated with minimal risk of transmission (Burchell AN).
About 15% of people aged 15-49 years of age are currently infected and more than 50% of sexually active men and women acquire genital HPV in their lifetime.
Approximately 7000 cases of cancer associated HPV genotypes 16 and 18, primarily anal, penile and oropharyngeal cancers occur in men annually in the US.
Associated with squamous cell carcinomas, adenocarcinomas, and dysplastic changes of the cervix, penis, vulva anus and vagina.
In men,HPV infection can cause genital warts, oenile intraepithelial neoplasia, and penile carcinomas.
In men most HPV infections are asymptomatic, and up to 705 are cleared within one year.
In men the median time to clearance of infection of HPV is 7.5 months, while the median time to clearance of high risk oncogenic HPV 16 is 12.2 months.
When HPV infections in men do not clear they manifest most commonly as genital warts.
Sexually transmitted HPV contributes to approximately 20,000 cases of invasive cancer each year in the United States, and cervical cancers make up about 50% of cases.
Aside from cervical cancers other cancers associated with HPV virus include vaginal, vulva, penis, anus, and oral cavity-oropharynx.
HPV 16 and HPV 18 are responsible for the development of the majority of carcinomas arising from the cervix (greater than 90%), anus (greater than 90%), vaginal/volva (greater than 60%), and penis (50%).
Fewer than 25% of HPV-related cancers occur in males.
A major cause of anogenital cancers, especially among men who have sex with men.
Oncogenic types of HPV cause nearly all cases of cervical cancer and 90% of anal cancers.
More than 20 types isolated with cervical cancers.
Most females who have HPV infections clear it within 12 to 24 months.
Most infected patients are asymptomatic and transient.
Most HPV infections clear spontaneously, but persistent infection is necessary to cause cervical cancer.
The presence of HPV was strongly correlated with non-melanoma skin cancers.
Ultraviolet radiation, as well as immunosuppression, lead to skin cancer, and that chronically sun-exposed skin is more likely to have HPV.
75% of tested non-melanoma skin cancer biopsies exhibited at least one of three viruses: HPV, Merkel cell polyomavirus, and Epstein-Barr virus(Baez et al).
Only 38% of non-cancerous skin biopsies, however, positive for these viruses.
HPV detection was common in non-melanoma skin cancers, 43%, but was nearly absent in non-cancerous biopsies.
Furthermore, Merkel cell polyomavirus is correlated with sites of increased exposure to ultraviolet radiation.
Epstein-Barr virus is significantly linked to immunocompromise.
Ultimately, HPV was strongly associated with non-melanoma skin cancer, while Epstein-Barr virus and Merkel cell polyomavirus were associated with other risk factors.
It is suggested that oncogenic viruses may play a role in non-melanoma skin cancers.
Multiple studies have shown a correlation between viruses and non-melanoma skin cancer, particularly HPV, squamous cell carcinoma, and basal cell carcinoma.
HPV vaccine is available for the prevention of cervical cancer, and this vaccine could possibly decrease non-melanoma skin cancer development in at-risk populations.
Progression from HPV infection to precancerous abnormal cell growth to cervical cancer is a slow process that takes decades to complete.
HPV infection occurs most often in 15-24 year olds, and cervical cancer occurs most often in women aged >40 years.
Approximately 30-40 types regularly identified in the lower genital tract.
An epithliotropic virus, meaning that to complete its growth cycle it must reside in the differentiating keratinocytes of the skin and anogenital and orophayrngeal mucosa.
HPV strains achieve carcinogenicity through degradation or inactivation of p53 and Rb via the products of eraly genes E6 and E7, respectively.
Some HPV infections persist, and women with persistent infection have an increased risk of developing cervical intraepithelial neoplasia Grade 3 (CIN3) the precursor to cervical carcinoma.
Cofactors associated with the development of CIN3 or carcinoma from oncogenic HPV infection are long duration of the use of oral contraceptives, multiparty, smoking abuse, host immune dysfunction, and other sexually transmitted diseases.
95% of cervical cancer specimens have HPV DNA detected.
Types are assigned numerical designation when their sequence has been established and a comparison with previous types indicates less than 90 homology in the L1, E6 and E7 regions of the virus.
Rates of infection in young sexually active females range from 19-46%.
Estimated to be the most common sexually transmitted infection in the U.S.
HPV DNA testing is more reproducible than cytological screening and colposcopy for detection of cervical precancerous and cancer lesions.
The presence of abnormal keratinocytes is a characteristic feature of productive HPV infection.
The risk of perinatal HPV transmission to the oropharyngeal mucosa of the neonate is low for mothers with latent infections or genital warts.
Patients with genital warts are an increased risk for anogenital malignancy.
Infection with HPV is the primary cause of cervical malignancy, though most patients with HPV-infected cervices have a benign outcome.
Annual screening and Pap testing are mandatory for female patients with genital warts.
As many as 90% of cervical cancers are caused by HPV infection of the cervix.
Comparison of the biopsy results with those from the Pap and cobas HPV tests showed that the HPV test is effective even when used alone.
The two common methods for HPV DNA testing are the Hybrid Capture II (HC II) and the polymerase chain reaction (PCR) enzyme immunosorbent assay.
HPV DNA testing is the preferred evaluation in the treatment of women whose Pap test results show atypical squamous cells of undetermined significance (ASC-US).
HPV DNA testing can be used alone for primary cervical cancer screening in women aged 25 years or older.
The test, the cobas HPV Test, detects DNA from 14 high-risk HPV types in cervical cell samples, and a positive test for HPV type 16 or 18 is considered an indication for a colposcopy.
A positive test for any of the 12 other high-risk HPV types is considered an indication for a Papanicolaou test, in order to determine the need for colposcopy.
The acetic acid test: soaking acetic acid into suspicious lesions can enhance the degree of suspicion in lesions.
The acetic acid test involves applyinga 3-5% acetic acid–moistened gauze pad for 5-10 minutes on suspected lesions of the cervix.
False-positive results are common with the acetic acid test and can result from anything that causes parakeratosis including: candidiasis, psoriasis, lichen planus, healing epithelium, sebaceous glands.
The acetic acid test is used in conjunction with colposcopy to examine cervical lesions.
The test is reserved only for suspicious lesions and should not be used for routine screening.
Tissue biopsy can be used to confirm HPV infection if the diagnosis is uncertain.
Infected cells exhibit a high degree of nuclear atypia.
A negative HPV DNA is a reassuring finding that premalignant or malignant disease does not exist.
Most patients with HPV infection do not develop cervical cancer.
Types 2 and 4 commonly cause warts on fingers and type 1 causes plantar warts.
Non-oncogenic types six and 11 cause approximately 340,000 cases of genital warts in the United States each year (Hoy T et al).
HPV types 6 and 11 cause grave in 90% of genital networks and most cases of recurrent respiratory papillomatosis.
Type 16 associated with carcinoma of the cervix.
Types 16 and 18 account for 70% of cervical cancers.
Types 16 and 18 account for 70% of all cervical cancer and adenocarcinoma in situ, cervical intraepithelial neoplasia (CIN) type 3, vulvar intraepithelial neoplasia (VIN) types 2 and 3, vaginal intraepithelial neoplasia (VaIN) types 2 and 3, and 50% of all cases of CIN2.
Types 6 and 11 account for 35%-50% of all CIN1, VIN1, and VaIN1cases, as well as 90% of all genital warts.
Types 16,18, 31 and 45 most common high risk types associated with cervical cancer.
Type16 accounts for 60% and type 18 accounts for 10-20% of cervical cancers.
HPV vaccine using the L1 virus like particle for HPV 16, and 18 is a preventative for cervical cancer.
Types 6 and 11 account for 90% of genital warts.
95% of cervical cancer specimens have HPV DNA detected.
Type 16 a risk factor for head and neck cancer.
Types 5 and 8 associated with skin wart infections that can progress to squamous cell carcinoma.
Approximately 30 types of HPV can cause sexually transmitted infections of the oral and anogenital areas.
Oral HPV infection among men and women aged 14-69 is approximately 7%, markedly lower than prevalence of genital HPV infection.
Oral HPV infection more common in men, with prevalence men:women 10.1%:3.6%.
Oral HPV infection bimodal with peaks at 30-34 years and 60-64 years.
Oral HPV-16 infection detected in 1% of men and women in the US.
Oral HPV infection prevalence is as high as 20% among those with more than 20 lifetime sexual partners, and among current smokers of more than 20 cigarettes daily.
Type 16 involved with oropharyngeal squamous cell carcinoma.
The incidence of or oral pharyngeal cancers will exceed that of cervical cancer by the next decade.
Human papilloma virus (HPV)-type 16 integrates into oropharyngeal tumor cell nuclei.
E6 and E7 proteins, manipulate cell pathways to support the differentiation dependent in infectious cycle.
These proteins promote cellular proliferation in the lower levels of the epithelia allowing the proliferation of cells with genetic instability, induce telomerase expression, and eventually lead to cancer.
Human papilloma virus 16 subtype genome exists of 2 oncogenes, E6 and E7.
E6 oncoprotein results in destruction of the p53 tumor suppressor preventing programmed cell death.
E7 oncoprotein results in the destruction of the retinoblastoma (Rb) tumor suppresor protein.
Most oropharyngeal squamous cell cancers produce specific HPV proteins.
Oropharyngeal tumors in nonsmokers disproportionately infected with HPV.
Patients with HPV positivity and squamous cell cancer of the oropharynx have multiple sex partners and frequently engage in oral-genital relations.
Pap smears typically normal in patients infected with HPV.
Pregnant women infected with human papillomavirus (HPV) may be at increased risk for miscarriages and preterm deliveries.
Mothers who have HPV are almost twice as likely as those who are not infected to have premature rupture of membranes and 50% more likely to have preterm deliveries.
Women with HPV are also more than twice as likely to experience a miscarriage or stillbirth.
Higher HPV infection rates have been reported in pregnant women. Anogenital warts, which appear as flat, papular, or Cauliflower like growths, are usually diagnosed on the basis of clinical exam.
Recurrent respiratory papillomatosis usually manifests is hoarseness and strider.
Most general HPV infection is diagnosed on the basis of HPV testing as part of a screening for cervical cancer.
Treatments:
Medication treatments of HPV disease are applied topically on cutaneous surfaces.
Two broad categories of medications are effective in treating HPV disease:
Immune response modifiers, and Cytotoxic agents.
Immune response modifiers: imiquimod and interferon alfa and are primarily used in treatment of external anogenital warts or condylomata acuminata.
Cytotoxic agents:include the antiproliferative drugs, podophyllin, and 5-FU, as well as the chemodestructive or keratolytic agents salicylic acid, trichloroacetic acid (TCA), and bichloracetic acid (BCA).
The keratolytic agents are the only agents that are recommended for treatment of nongenital cutaneous warts.
Imiquimod is a powerful cytokine inducer that stimulates production of interferon alfa, tumor necrosis factor, interleukin (IL) – 1, IL-6, and IL-8.
Application of imiquimod 5% cream can result in complete resolution of genital warts in up to 50% of patients.
Interferon alfa has been used for the treatment of genital warts: Topical, intralesional, and systemic therapy.
Interferon alfa may be produced either through recombinant DNA technology or from pooled human leukocytes.
Interferon alfa has potent immunomodulatory, as well as direct antiviral, effects.
Interferon alfa is used for intralesional treatment of external anogenital warts and condyloma acuminatum.
For the treatment of external anogenital warts and condyloma acuminatum
local injection of interferon appears to be more effective than systemic injection.
Interferon for the treatment of genital warts associated with a complete response rate of 45%, with a 21% recurrence rate.
Interferon side effects include: flulike symptoms, fatigue, and pain.
Interferon is contraindicated in pregnancy.
Podofilox gel or solution is an antimitotic agent is either chemically synthesized or purified from naturally occurring podophyllin resin.
Podofilox is used in the treatment of external genital warts or condyloma acuminatum.
Podophyllin, contains the active agent podophyllotoxin, which is a cytotoxic agent that arrests mitosis in metaphase.
It is a physician-applied medicine used in the treatment of external genital warts and condyloma acuminatum.
((Podophyllin)) can causes tissue injury but also can be absorbed systemically and cause neurologic toxicity.
Deaths have occurred with the use of podophyllin on perianal warts.
Increased surface area of the lesions increases the absorption of the drug.
Podophyllin is contraindicated in pregnancy
