 Nonmalignant disease altering the mononuclear phagocytic system with histiocytes proliferation and prominent phagocytosis.
Nonmalignant disease altering the mononuclear phagocytic system with histiocytes proliferation and prominent phagocytosis.
HLH is a rare syndrome caused by defects, either inherited or acquired, in cytotoxic T lymphocytes and/or natural killer cells leading to an uncontrolled inflammatory response by activated macrophages.
Primary hemophagocytic lymphohistiocytosis is a rare syndrome characterized by immune dysregulation and hyper inflammation, that manifests in infancy and is associated with a high mortality.
A disorder of pathological activation of the immune system and it often is fatal is not properly recognized and managed.
Primary disease is a rare, autosomal recessive disorder of infancy either familial or sporadic.
Secondary disease associated with infection, malignancy, immunosuppression CAR-T cell therapy, and fat overload.
It can be diagnosed in adults due to underlying infection, auto immune disease, and malignant condition.
Life threatening syndrome with extreme inflammation due to an uncontrolled immune response.
Unrestrained and exaggerated inflammatory reactions.
Associated with ineffective immune response.
When hemophagocytic lymphohistiocytosis is associated with the setting of a rheumatological disease it is called macrophagevactivation syndrome.
Uncontrolled activation of the immune system lead to systemic inflammation, cytokine storm, and ultimately multiorgan failure.
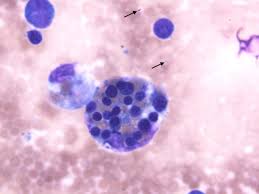
Widespread infiltration of lymphocytes and histiocytes, leading to hemophagocytosis.
Characterized as primary, familial, or secondary, acquired.
Familial disease occurs in infants and young children with a family history of HLH, or an underlying genetic defect with dysfunctional cytotoxic T lymphocyte cells, and natural killer (NK) cells.
Acquired HLH occurs in adults due to infectious, malignant or autoimmune disorders.
The most common conditions associated with HLH are malignancy, at about 50%, infections at 30%, auto immune disorders 10%, and idiopathic disease at 10%.
Occurs in an estimated 12-17% of cases of adult onset Still disease.
Lymphoproliferative disorders of the B and T cell origin are the most common causes of secondary HLH accounting for 68% of cases over the age of sixty years, followed by infections at 26%, and autoimmune disorders at 6%.
Clinical criteria required for the diagnosis involves five of the eight following criteria:
Fever
Splenomegaly
Cytopenia of two or more cell lines
Hypertriglyceridemia and or hypofibrinogenemia
Hematophagocytosis in bone marrow/lymph nodes/spleen
Low or absent NK-cell activity
Ferritin greater than 500 mcg/L
Soluble CD25 (IL 2 receptor) activity of greater 2400 units per mL.
Interferon gamma inhibits lipoprotein lipase which increases triglyceride levels.
Secretion of plasminogen activator by activated macrophages causes increased plasmin levels, hyperfibrinolysis, and decreased fibrinogen.
Ferritin production is increased by the macrophage enzyme heme oxygenase enzyme.
Elevated ferritin levels, is a relatively consistent findings in HLH adults.
Interleukins 1 and 6 are increased and produce fever and soluble IL-2 receptor increases in response to activation of Th1 cells.
Organ infiltration of the liver and spleen account for hepatosplenomegaly and neurological symptoms are a result of activation of lymphocytes in histiocytes.
Neurologic symptoms may include visual problems, seizures, irritability, altered mental status and may occur in up to 37% of patients.
Clinical features include fever, multi organ dysfunction, CNS issues.
HLH can be primary owing to genetic defects involving cytotoxic T cells and natural killer cells or secondary induced by viral infections, and autoimmune disorders and is usually associated with liver injury.
Pleocytosis and hematophagocytosis typically present in CSF fluid.
5-year survival in children is about 54%.
In an adult study of 250 adult patients the median age was 49 years, median survival 2.1 months for the entire group (Parikh, SA et al).
In the above study median survival is 1.4 months with malignant associated disease.
In the presence of malignancy or hypoalbuminemia the prognosis is poor.
Treatment of adult HLH is based on correcting the underlying precipitating factor and the associated hyper inflammatory response.
On patients with infection associated HLH can be treated adequately for the underlying infection.
The addition of immunosuppressive and corticosteroids. cyclosporine or intervenous immunoglobulins are consider in patients with severe hyperinflammatory responses.
In EBV associated HLH etoposide based treatment has shown improvement in outcomes, have the addition of rituximab.
Emapalumab (Gamifant) is the first treatment specifically approved for primary hemophagocytic lymphohistiocytosis.
A combination of liposomal doxorubicin, etoposide , and high-dose methylprednisone had an overall response rate of 76%: median survival only seven months.
