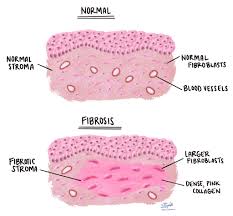
 Fibrosis refers to the pathologic accumulation of extracellular matrix.
Fibrosis refers to the pathologic accumulation of extracellular matrix.
Fibrosis is the final outcome of common inflammatory, immuno mediated and metabolic diseases.
Fibrosis accounts for up to 45% of all deaths in the industrialized world.
Tissue injury of any organ results in cellular and molecular responses that culminate in tissue fibrosis.
Scarring, or fibrosis is a response to tissue injury throughout the body.
More than 40% of of all deaths are attributable to scarring of the heart, liver, lung, kidney, bone marrow, or skin.
Scarring, or fibrosis, over a prolonged period of time leads to cellular dysfunction and organ failure.
Fibrosis impairs tissue function over time.
There are fibrogenic cells within each tissue: resident perivascular mesenchymal cells, pericytes and fibroblasts, which have the ability to transform or activate through tissue injury into contractile fibrogenic cells that secrete scar molecules, primarily interstitial collagen and specialized glycoloproteins, to create a dense network that can interfere with organ function.
There are four phases of fibrotic response: first the initiation of the response by the primary injury to the organ, second phase is the activation of effector cells, the third phase is elaboration of extracellular matrix, and the fourth phase is the deposition of extracellular metrics promoting progression to fibrosis and in the organ failure.
Fibrosis is a complex process involving multiple different types of cells with involvement of specific molecular pathways.
Cellular constituents include macrophages, T cells, epithelial cells, fibrogenic effector cells, endothelial cells, fibroblasts, myofibroblasts, bone marrow cells, fibrocytes.
Transforming growth factor beta pathway (TGF-Beta) is important in the development of all types of fibrosis..
There are presently no approved therapies to reverse fibrosis.
CAR-T is presently being investigated.
