 Extracorporeal cardiopulmonary resuscitation (ECPR) is a method of cardiopulmonary resuscitation (CPR) that passes the patient’s blood through a machine in a process to oxygenate the blood supply.
Extracorporeal cardiopulmonary resuscitation (ECPR) is a method of cardiopulmonary resuscitation (CPR) that passes the patient’s blood through a machine in a process to oxygenate the blood supply.
It consists of the implantation of venoarterial extracorporeal membrane oxygenation during cardiac arrest.
It was initially intended to facilitate blood flow and oxygen delivery to the body during operation on a non-beating heart.
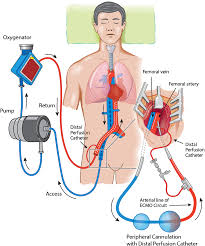
Patients undergo cannulation of the venous and arterial systems to provide perfusion support, extracorporal oxygenation, and temperature management as a means of organ preservation, while the return of spontaneous circulation is pursued, often with the use of coronary angiography and intervention.
A portable extracorporeal membrane oxygenation (ECMO) device is used as an adjunct to standard CPR.
A patient who is deemed to be in cardiac arrest refractory to CPR has percutaneous catheters inserted into the femoral vein and artery.
By attaching an ECMO device to a person who has acutely undergone cardiovascular collapse, the maintenance of end-organ perfusion can be achieved while assessing the potential reversal of causal pathology, with the goal of improving long-term survival and neurological outcomes.
During ECPR blood is removed from a central vein, such as the inferior vena cava, and circulated through a membrane oxygenator where carbon dioxide is removed, and oxygen is added before the blood is returned through the femoral artery into the aorta.
Blood delivery from the aorta facilitates organ, perfusion, including coronary and cerebral perfusion.
ECPR allows organs such as the heart and lungs to recover from injury related to cardiac arrest, providing time for reversible causes to be treated.
Oxygenation and perfusion can be maintained with an ECMO device in patients undergoing cardiovascular collapse, as with cardiopulmonary bypass.
In the setting of cardiac arrest, ECPR involves percutaneous cannulation of a femoral vein and artery.
The device maintains circulation until an appropriate recovery is made.
The theory behind this invasive approach is that the artificial restoration of oxygenation and end-organ perfusion allows treating physicians more time to mitigate and reverse pathology which contributes to cardiac arrest and refractory shock.
The likelihood of return of spontaneous circulation and eventual discharge from hospital, after ten minutes of CPR falls significantly.
Once circulation is established, the patient is able to be transferred, for further investigation and intervention, to facilities such as a cardiac cath lab and an intensive care unit.
Extracorporeal life support (ECLS) systems are portable and utilize percutaneous access as opposed to catheters which are surgically inserted into an open chest.
The first access enters the femoral vein at the groin and is extended superiorly to the right atrium.
The second line enters the ipsilateral or contralateral femoral artery and advanced to the distal aorta.
Deoxygenated blood is removed from the right atrium prior to being pumped through the ECLS device where it is oxygenated and returned as retrograde flow to the distal aorta
ECPR is largely viewed as a rescue therapy, which is initiated in patients in cardiac arrest or profound circulatory shock, for whom all conventional therapies have been exhausted and death without further support is imminent.
Indications
The patient was generally healthy prior to the arrest.
Overall goals of therapy are curative: The cause of the cardiac arrest is thought to be reversible with an available medical or surgical intervention.
Out-of-hospital cardiac arrest which is refractory to standard advanced cardiac life support (ACLS) treatment.
Criteria for ECPR
The cardiac arrest is likely to be of primary cardiac or respiratory cause.
The cardiac arrest was witnessed
Chest compressions were commenced within 10 minutes
The cardiac arrest duration has been < 60 minutes
The patient is aged between 12–70 years
There are no major co-morbidities that would preclude return to independent living
The patient is profoundly hypothermic (<32 °C) due to accidental exposure
The patient has taken a significant overdose of a vaso-active drug(s)
Any other cause where there is likely to be reversibility of the cardiac arrest if an artificial circulation can be provided.
Patients with in-hospital cardiac arrest, which is refractory to standard, advanced cardiac life support (ACLS) treatment and in whom the cause may be reversible.
Any other cause where there is likely to be reversibility of the underlying condition if an artificial circulation can be provided.
No precise list of contraindications has been established.
There is range of circumstances in which the use of ECPR would be inappropriate: Premorbid severe neurological impairment including stroke, dementia and traumatic brain injury.
Shock secondary to sepsis or hemorrhage.
Chest compressions not initiated within 10 minutes of commencement of cardiac arrest
Total arrest time greater than 60 minutes.
No realistic prospect of reversal of underlying cardiac or respiratory pathology.
Advanced age precludes an extended ICU admission requiring mechanical support.
The risk associated with the initial process of connecting a patient to an extracorporeal life support device is potentially exacerbated by the emergent nature of ECMO CPR.
Complication of the initial application and from remaining on the extracorporeal oxygenation circuit include:
Leg ischemia
Bleeding
Pneumonia
Sepsis
Acute kidney injury
Pressure areas
Initiating ECPR
Once successful cannulation is confirmed, 5000 units of intravenous heparin is administered.
The cannula are attached to an ECMO circuit with blood flow targets of 3Lmin−1 and oxygen blood flow of 3L min−1.
Mean arterial perfusion pressures of 70mmHg are targeted.
Once stabilized on the ECMO circuit, further management of causal pathology is performed.
The maintenance of therapeutic hypothermia is arrest scenarios at a a target temperature of 33°C is maintained for the first 24 hours following commencement of ECMO, with gradual rewarming occurring thereafter.
Due to the very nature of ECPR, randomised control trial are largely unfeasible.
In the pediatric population the indication for ECPR is primarily due to cardiac collapse, often associated with congenital pathology.
With adults ECMO is only indicated if reversal of the pathology is feasible.
The survival rate for individuals who have undergone ECPR for cardiac arrest is approximately 30%.
Approximately 25% of patients experience bleeding and approximately 5% experience limb ischemia distal to the femoral arterial cannula.
ECPR is more effective than conventional. CPR in the treatment of cardiac arrest based on randomized trials.
