 Esophagogastric junctional adenocarcinoma (EGJ) is a cancer of the lower part of the oesophagus with a rising incidence in Western countries.
Esophagogastric junctional adenocarcinoma (EGJ) is a cancer of the lower part of the oesophagus with a rising incidence in Western countries.
This disease is often linked to Barrett’s oesophagus.
The incidence of EGJ adenocarcinoma is rising rapidly in Western countries especially in recent decades, in contrast to the declining frequency of distal gastric adenocarcinoma.
Treatment options for adenocarcinomas involving the esophagogastric junction are limited and the overall prognosis is extremely poor, with a five-year survival rate of approximately 30% with surgery alone.
Risk factors for EGJ adenocarcinoma.
The biggest risk factors include gastroesophageal reflux disease (GERD) and Barrett’s oesophagus.
Other risk factors include smoking, with a twofold-increase, and obesity.
The clinical features of EGJ adenocarcinoma are variable depending on the extent of the tumor.
Early stages are oftentimes asymptomatic or have difficulty swallowing.
More advanced stages can present with signs and symptoms of anemia, especially iron deficiency anemia from chronic gastrointestinal bleeding, weight loss, cervical adenopathy, hoarseness or change in voice, and progressive difficulty with swallowing, initially with solid foods and then with liquids.
Distant metastases typically occur in the liver, lungs, bones, and adrenal glands and can manifest with symptoms typical of involvement with these sites.
The diagnostic workup for EGJ adenocarcinoma usually involves performing an endoscopy with endoscopic biopsy.
Accurate staging of tumor extent and involvement of surrounding tissue or distant metastases is critical to establishing a prognosis, and is usually guided by endoscopic ultrasound, computed tomography scans, and/or positron emission tomography scans to establish the extent of disease.
Additionally, genetic analysis of the tumor may yield mutations that may be clinically significant
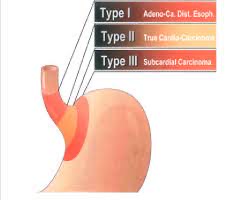
The Siewart classification system is a classification scheme used for EGJ adenocarcinomas.
A Type I tumor, located between 5 and 1cm proximal to the EGJ, is an adenocarcinoma that typically arises from an area of intestinal metaplasia of the esophagus and can infiltrate the EGJ from above.
A Type II tumor, located between 1cm proximal and 2cm distal to the EGJ, is a true adenocarcinoma of the gastric cardia.
A Type III tumor, located between 2 and 5 cm distal to the EGJ is a subcardial gastric carcinoma that typically infiltrates the EGJ from below.
EGJ adenocarcinoma is a highly mutated and heterogeneous disease.
Microsatellite instability (MSI) can be observed and coincides with an elevated number of somatic mutations.
Chromosomal instability high tumors account for 50% of all esophagogastric cancers and nearly 70% of GE junction tumors.
Chromosomal instability is a dynamic process in which chromosomes undergo high rates of misregulation during cell division, creating a large number of fragile micronuclei, which, upon rupture, lead to the presence of pathogenic DNA.
HER2play a significant role signaling in initiating and sustaining chromosomal instability via defective cell cycle control.
HER2 positive Esophagogastric cancer accounts for approximately 20% of such cases.
Potentially actionable coding mutations have been identified in 67 genes, including those in CR2, HGF, FGFR4 and ESRRB.
TP53, SYNE1, and ARID1A are among the most frequently mutated genes.
Notably, up to one third of EGJ adenocarcinomas have been found to have human epidermal growth factor receptor 2 (HER2) overexpression or amplification, which may be targetable with trastuzumab, conferring a modest survival benefit based on initial clinical trials.
Studies show that the use of trastuzumab Deruxetan as a second line therapy in patients with HER2 positive advanced gastric or gastroesophageal junction cancer.
Treatment:
There is no established consensus on treatment approaches for EGJ adenocarcinoma.
The mainstay of treatment is surgical resection, guided by the Siewart classification system, followed by adjuvant chemotherapy for advanced disease.
The addition of checkpoint inhibitors to chemotherapy improved response rate in patients with advanced gastric or gastroesophageal junction adenocarcinoma: may become frontline treatment.
Monoclonal HER2 antibody therapy is standard care for metastatic disease.
Among patients with unresectable, locally, advanced or metastatic gastric/gastroesophageal junction, adenocarcinoma treated with first line chemotherapy and sintilimab (a PD-L1inhibitor) significantly improved overall survival for all patients and for patients with a combined positive PD-L1 score of 5 or more compared with placebo.
HER2 monoclonal antibody and checkpoint inhibitor therapy may be most beneficial.
