Rare chronic disorder of esophageal motor function affecting 1 in 100.000 population per year.
Patients typically complain of dysphagia, regurgitation and chest pain.
A primary motor disorder of the esophagus characterized by incomplete lower esophageal sphincter relaxation during swallowing.
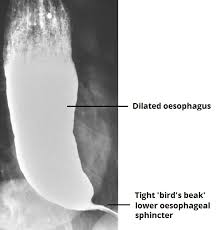
Primary abnormalities are absence of esophageal body peristalsis, and failure of the lower esophageal sphincter to relax on swallowing.
Symptoms may be caused by diseases such as gastroesophageal reflux, malignancy, mechanical instruction with strictures, rings, diverticuli and achalasia and other motility disorders.
Etiologies include: parasitic, autoimmune, neurodegenerative, and possibly viral causes.
Physiological abnormality thought to be secondary to degeneration of the esophageal myenteric plexus, predominantly affecting inhibitory ganglionic neurons.
Esophageal motor function is a balance of stimulatory and inhibitory intrinsic neural activities.
Acetylcholine mediation is stimulatory on the motor function of the esophagus and nitrogen oxide and vasoactive intestinal peptides are inhibitory.
Achalasia is a motor disorder of the esophagus characterized by decrease in ganglion cell density in the myenteric plexus.
In achalasia there is a selective degeneration of ganglion cells in the myenteric plexus of the lower esophageal sphincter and esophageal body, leading to impaired release of the inhibitory neurotransmitters nitric oxide and vasoactive intestinal peptide.
This lack of inhibitor activity leads to unopposed excitatory or cholinergic activity and aperistalsis of the esophagus and incomplete relaxation of the lower esophageal sphincter.
When dysphasia symptoms persist, endoscopy should be performed to evaluate for mechanical obstruction or inflammatory processes:if these are not found achalasia is considered in the diagnostic differential.
Liquids can accumulate and pool above an non-relaxing lower esophageal sphincter.
Not a curable process and goal of treatment is palliation by decreasing obstruction at the lower esophageal sphincter.
Treatment options include drug agents, including endoscopic injection of botulinum toxin a into the esophageal sphincter, pneumatic dilation of the lower esophageal sphincter and surgery with division of the smooth muscle of the lower esophageal sphincter.
In the only randomized trial comparing the outcomes of pneumatic dilation and surgical myotomy good long term results were seen in 65% and 95%, respectively.
Endoscopic pneumatic dilation is the most commonly performed treatment.
1-3% of endoscopic pneumatic dilation procedures is complicated by perforation.
Response to medications is poor and use of botulinum toxin injection is transient.
Laparoscopic myotomy of the distal esophagus and gastric cardia with antireflux anterior partial fundoplication is considered the treatment of choice.
Laparoscopic myotomy of the distal esophagus combined with an anti-reflux procedure offers a more permanent solution for patients, with the success rate of 80-90%.
Laparoscopic myotomy of the distal esophagus is invasive and is associated with severe complications including colon perforation at 4-10%, bleeding, or infection.
Laparoscopic myotomy of the distal esophagus he is generally utilized for patients who do not respond to pneumatic dilation.
Peroral endoscopic myotomy has been shown in a randomized trial to have fewer complications, and a better success rate than a pneumatic dilation group and may should be the initial treatment option for patients with achalasia (PondsFA).
Dysphagia or chest pain recurs in approximately 10% of patients after myotomy.
In a randomized trial peroral endoscopic myotomy was non-inferior to laparoscopic myotomy In controlling symptoms of achalasia at two years (Werner YB).
