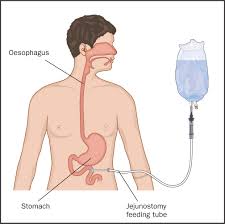
 Enteral nutrition is the following is providing essential entrance through an enteral tube to prevent or treat disease related malnutrition in patients who are unable to continue adequate nutrients by mouth.
Enteral nutrition is the following is providing essential entrance through an enteral tube to prevent or treat disease related malnutrition in patients who are unable to continue adequate nutrients by mouth.
Provides no advantage in preservation of gut barrier function, development of infectious complications, morbidity or mortality when energy and nitrogen intakes are similar.
Associated with fewer complications than parenteral nutrition and is less expensive to use.
Its use often, however, does not achieve caloric targets.
The main reason of non-use of EN is gastrointestinal intolerance ascribed to gastroparesis, with increased gastric volume, gastroesophageal reflux, regurgitation, vomiting, and risk of aspiration and ventilator associtrd pneumonoa.
Underfeeding critically ill patients is associated with weakness, infection, increased duration of mechanical ventilation and death.
Because patients cannot eat normally, artificial nutrition is often provided in patients with acute lung injury and with long duration of mechanical ventilation.
Enteral nutrition targeting full caloric needs is advocated over parenteral nutrition during mechanical ventilation.
Enteral nutrition is used in about 5% of malnourished hospitalized patients in the US.
Enteral nutrition is considered in patients with critical illness, dysphasia, neurologic, disease, gastrointestinal, or liver disease, cancer, cystic fibrosis, COPD and kidney disease.
Enteral nutrition is associated with improved clinical outcomes, fewer infections, shorter duration of mechanical ventilation, and lower mortality rates for patients receiving a higher percentage of calculated caloric needs.
Intermittent or continuous feedings have similar outcomes in the number of stools per day and the likelihood of diarrhea or vomiting in critically ill children in pediatric intensive care units.
Vomiting occurs in approximately 6-12% of adult patients treated with continuous infusion nutrition.
The results of intermittent or continuous infusion feedings on the incidence of diarrhea have resulted in inconsistent results.
Early feeding with intraoperative jejunostomy is the pref2242ed method for nutritional support of severely injured patients having surgery for multiple trauma.
Compared to parenteral nutrition results in a statistically reduced risk for infectious complications, pancreatic infections and mortality (Petrov).
Enteral nutrition use, as compared to parenteral nutrition in ICU patients is preferred when patients are able to do so.
Enteral nutrition contraindicated with diffuse peritonitis, intestinal obstruction, early stages of short bowel syndrome, paralytic ileus, intractable vomiting, severe gastrointestinal bleeding, severe diarrhea, high output fistulae, severe intestinal hemorrhages, intestinal ischemia, shock, and malabsorption syndromes.
Relative contraindications to use include pancreatitis and enterocutaneous fistulae.
A meta-analysis of intention-to-treat trials comparing enteral with parenteral nutrition in critically ill patients, revealed a reduction in mortality among patients receiving parenteral nutrition (Simpson F).
In the above studies, if enteral nutrition was started within 24 hours of ICU admission no significant benefit was apparent for parenteral nutrition, and significant increases of infection occured in the parenteral nutrition group.(Simpson F).
13 randomized trials revealed that enteral nutrition in critically ill adult patients was associated with significant reductions in infectious complications compared to parenteral nutrition without a difference in mortality (Gramlich L).
Enteral nutrition in patients with mechanical ventilation indicate improved clinical outcomes, fewer infections, shorter duration of mechanical ventilation and lower mortality.
Hypocaloric feeding, or permissive underfeeding may result in shorter ventilation and improve mortality.
Trophic feedings, minimal amounts of enteral feedings, have beneficial effects in preserving intestinal epithelium, stimulating secretion of brush border enzymes, enhancing immune functions, preserving epithelial cellular junctions, and preventing bacterial translocation, despite not meeting daily calorie requirements.
In a randomized study with acute lung injury patients on mechanical ventilation receiving trophic versus full enteral nutrition: there was no difference in ventilator free days, 60 day mortality, or infectious complications but was associated with less gastrointestinal intolerance (EDEN randomized trial.
