 Technique for surveillance of cardiac allograft rejection, and to evaluate dilated and restrictive cardiomyopathies.
Technique for surveillance of cardiac allograft rejection, and to evaluate dilated and restrictive cardiomyopathies.
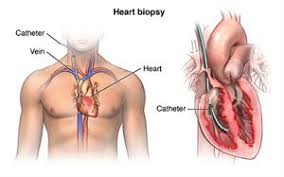
Endomyocardial biopsy (EMB) is an invasive procedure used routinely to obtain small samples of heart muscle, primarily for detecting rejection of a donor heart following heart transplantation.
Preferred access is the right internal jugular vein, although the right femoral vein and artery can be the access to the right and left ventricle, respectively.
Bioptomes achieve biopsy.
A bioptome is used to gain access to the heart via a sheath inserted into the right internal jugular or less commonly the femoral vein.
A bioptome is a small pincer-shaped cutting/grasping instrument used in medicine for taking endomyocardial biopsy specimens of the heart muscle following heart transplantation in rejection monitoring and for diagnosing some diseases of the heart.
Guidance and confirmation of correct positioning of the bioptome is made by echocardiography or fluoroscopy.
Monitoring during the procedure consists of performing ECGs and blood pressures.
A heart biopsy, also called myocardial biopsy or cardiac biopsy.
Refers to an invasive procedure to detect heart disease that involves using a bioptome to obtain a small piece of heart muscle tissue for analysis.
Used for: evaluation or confirmation of the presence of rejection after heart transplant.
Diagnose myocarditis or certain other cardiac disorders such as cardiomyopathy or cardiac amyloidosis.
A plastic introducer sheath is inserted through a small incision and into a blood vessel in the neck, and a bioptome is inserted through the sheath and threaded to the right ventricle.
The bioptome is used to obtain samples about the size of the head of a pin, of the heart muscle.
The procedure takes about 30 to 60 minutes.
Monitoring during the procedure includes performing ECGs and blood pressures.
Because the right ventricular wall is then, biopsy specimens from this area are dangerous, and should be taken from the interventricular septum.
In a study of more than 200 biopsies by echocardiography or fluoroscopic guidance myocardial perforation occurred in fluoroscopic 1.7% of cases, and right ventricular perforation occurred in 3.3% of trans femoral biopsies guided by echocardiography in 90 patients (Blomstrom-Lundqvist C et al, Han J et al).
Associated with acute complications less than 1% of cases using flexible bioptomes.
Overall complication rate less than 6% in most studies.
Complications include hematoma, arrhythmias of transient nature, transient RBBB, tricuspid regurgitation, and pulmonary embolism.
Serious complications include perforation of the heart with pericardial tamponade, haemopericardium, AV block, tricuspid regurgitation and pneumothorax.
Risk of death 0.1% and a 0.25% risk of cardiac perforation.
Less commonly the left ventricle can be biopsied via the femoral artery.
The accuracy of diagnosis depends on whether the correct site is biopsied, especially with myocardial inflammation or fibrosis.
EMB has a low risk of less than 1% of complications when performed by an experienced team.
Possible complications: rupture of the right intraventricular septum, conduction block, arrhythmias, pneumothorax, tricuspid regurgitation, atrioventricular fistula, and pulmonary embolism.
Death is a rare complication.
Used to detect immediate cardiac transplant rejection, and is preferred for long-term rejection surveillance.
Sometimes to evaluate cardiomyopathy, some heart disease research and ventricular arrhythmias, or unexplained ventricular dysfunction.
Endomyocardial biopsy allows the detection of cell-mediated or antibody-mediated rejection and is recommended episodically during the first year after heart transplantation.
It has a role in the diagnosis of viral myocarditis and inflammatory myocarditis.
Cardiac perforation risk is small in heart transplants because the pericardial space is almost obliterated and any right ventricular perforation is contained by the pericardium.
With repeat endomyocardial biopsy scarring of the interventricular septum may occur and increased the difficulty in obtaining samples.
Patients who undergo repeated EMB are at risk for long-term complications, including coronary artery-to-right ventricular fistula, and tricuspid valve regurgitation.
EMB induced tricuspid regurgitation is associated with increased late mortality.
Neither two dimensional transthoracic echocardiography nor fluoroscopy guidance provides adequate chordae tendineae visualization and can be damaged by EMB.
Indicated procedure in young patients with myocarditis, and older patients with suspected infiltrative cardiomyopathy.
Monitoring during the procedure includes performing ECGs and blood pressures.
