Each year more than 320,000 people in US undergo CABG.
Coronary artery bypass graft surgery is the second most common method of coronary artery revascularization after percutaneous coronary intervention (PCI).
CABG surgery using a combination of venous and arterial conduits is often the preferred revascularization approach for patients with complex coronary artery disease who are good surgical candidates.
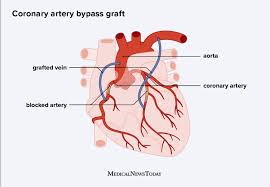
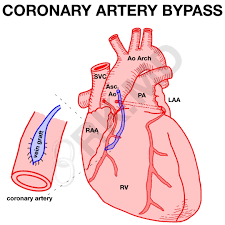
Coronary artery bypass surgery, also known as coronary artery bypass graft (CABG, cabbage) surgery, and heart bypass or bypass surgery, is a surgical procedure to restore normal blood flow to an obstructed coronary artery.
There are two main surgical approaches. In one, the left internal thoracic artery, LITA (also called left internal mammary artery, LIMA) is diverted to the left anterior descending branch of the left coronary artery.
The left internal mammary artery is pedicled and not detached from the origin.
In the other process, a great saphenous vein is removed from a leg; one end is attached to the aorta or one of its major branches, and the other end is attached to the obstructed artery immediately after the obstruction to restore blood flow.
CABG is performed to relieve angina, prevent or relieve left ventricular dysfunction, and/or reduce the risk of death.
This surgery is usually performed with the heart stopped, necessitating the usage of cardiopulmonary bypass.
Two alternative techniques are also available, allowing CABG to be performed on a beating heart either without using the cardiopulmonary bypass, off-pump surgery, or performing beating surgery using partial assistance of the cardiopulmonary bypass, on-pump beating surgery.
CABG is often indicated when coronary arteries have a 50 to 99 percent obstruction.
The obstruction being bypassed is typically due to arteriosclerosis, which is characterized by thickening, loss of elasticity, and calcification of the arterial wall, most often resulting in a generalized narrowing in the affected coronary artery.
Atherosclerosis is characterized by yellowish plaques of cholesterol, lipids, and cellular debris deposited into the inner layer of the wall of a large or medium-sized coronary artery, most often resulting in a partial obstruction in the affected artery.
There is no survival benefit with bypass surgery vs. medical therapy in stable angina patients.
The benefits of CABG surgery when compared to medical therapy: prolongs survival not only in patients with 3-vessel disease but also with left main disease and 1- or 2- vessel disease with proximal LAD disease.
Bypass surgery does not prevent future myocardial infarctions.
Age per se is not a factor in determining risk vs benefit of CABG.
CABG guidelines:
Preferred treatment for:
Disease of the left main coronary artery (LMCA).
Disease of all three coronary arteries (LAD, LCX and RCA).
Diffuse disease not amenable to treatment with a percutaneous coronary intervention (PCI).
It is the preferred treatment with other high-risk patients such as those with severe ventricular dysfunction, low ejection fraction or diabetes mellitus.
Bypass surgery does not prevent future myocardial infarctions.
Age per se is not a factor in determining risk vs benefit of CABG.
Prognosis following CABG: successful grafts typically last 8–15 years.
CABG improves the chances of survival of patients who are at high risk, generally triple or higher bypass, though statistically after about five years the difference in survival rate between those who have had surgery and those treated by drug therapy diminishes.
Age at the time of CABG is critical to the prognosis: younger patients with no complicating diseases do better, while older patients can usually be expected to experience further blockage of the coronary arteries.
Veins that are used either have their valves removed or are turned around so that the valves in them do not occlude blood flow in the graft.
Left internal mammary artery grafts are longer-lasting than vein grafts: the artery is more robust than a vein and it is already connected to the arterial tree, needing only be grafted at one end.
Left internal mammary artery graft is usually grafted to the left anterior descending coronary artery (LAD) because of its superior long-term patency when compared to saphenous vein grafts.
CABG or stent placement is indicated when medical management with anti-angina medications, statins, antihypertensives, smoking cessation, and/or tight blood sugar control in diabetics, do not satisfactorily relieve ischemic symptoms.
Both PCI and CABG are more effective than medical management at relieving symptoms of angina, dyspnea, or fatigue.
CABG is superior to PCI for most of the patients with multivessel CAD.
The SYNTAX study found a 40% higher mortality in patient with 3-vessel coronary artery disease treated with PCI in comparison with CABG.
The Surgery or Stent (SoS) trial demonstrated CABG is superior to PCI in multivessel coronary disease.
The SYNTAX trial was a randomized controlled trial of 1800 patients with multivessel coronary disease, comparing CABG versus PCI using drug-eluting stents: rates of major adverse cardiac or cerebrovascular events at 12 months were significantly higher in the drug-eluting stents group (17.8% versus 12.4% for CABG.
There is a higher need for repeat revascularization procedures and more post-procedural myocardial infarctions in the PCI group with no difference in long-term survival.
Higher rates of strokes are seen in the CABG group.
Patients in New York state treated with CABG or percutaneous coronary intervention (PCI) demonstrated CABG was superior to PCI with drug eluting stents in multivessel coronary artery disease.
Patients treated with CABG had lower rates of death and of death or myocardial infarction than treatment with a coronary stent, and also had lower rates of repeat revascularization.
A meta-analysis with over 6000 patients showed that coronary artery bypass was associated with lower risk for major adverse cardiac events compared to drug-eluting stenting.
However, patients had a higher risk of stroke events.
A meta-analysis with over 4000 patient cases found hybrid coronary revascularization (LIMA-to-LAD anastomosis combined with percutaneous stents at other atherosclerotic sites) to have significant advantages compared with conventional CABG.
Postperfusion syndrome os a transient neurocognitive impairment associated with cardiopulmonary bypass.
Some studies shows the incidence of postperfusion syndrome initially decreased by off-pump coronary artery bypass, but with no difference beyond three months after surgery.
A neurocognitive decline over time has been demonstrated in people with coronary artery disease regardless of treatment and Studies suggests that longer term cognitive decline is not caused by CABG but is rather a consequence of vascular disease.
Loss of mental function is a complication of bypass surgery in the elderly.
The heart-lung blood circulation system employed during CABG, and the surgery itself release a variety of debris: parts of blood cells, tubing, and plaques.
Clamping and connecting the aorta to tubing, results in emboli that could block blood flow and cause mini strokes.
Other cardiac surgical factors related to mental damage may be events of hypoxia, high or low body temperature, abnormal blood pressure, irregular heart rhythms, and fever after surgery.
Complications of CABG:
Myocardial infarction due to embolism, hypoperfusion, or graft failure.
While remote ischemic preconditioning (RIPC) reduces the cardiac troponin T (cTnT) release measured at 72 hours after surgery and cardiac troponin I (cTnI) release measured at 48 hours and 72 hours after surgery.
RIPC does not reduce reperfusion injury in people undergoing cardiac surgery.
Late graft stenosis, particularly of saphenous vein grafts due to atherosclerosis causing recurrent angina or myocardial infarction.
Long-term patency of graft conduits is limited: saphenous vein grafts have a higher rate of failure than do arterial grafts.
3 to 12% of vein grafts fail before hospital discharge, 8 to 25% failing at one year, and 40 to 50% failing at 10 years.
Only the use of postoperative aspirin and statins have been shown in randomized trials to reduce saphenous vein graft failures.
Risk factors for early saphenous vein graft occlusion is related to procedural techniques: trauma to the venous conduit during harvesting or a size mismatch between the conduit and the target vessel: these mechanical issues serve as a nidus for thrombus formation that can lead to saphenous vein occlusion
The terms single bypass, double bypass, triple bypass, quadruple bypass and quintuple bypass refer to the number of coronary arteries bypassed in the procedure.
Left main coronary artery obstruction requires two bypasses, one to the LAD and one to the LCX.
A coronary artery may be unsuitable for bypass grafting: small (< 1 mm or < 1.5 mm), heavily calcified, or located within the heart muscle rather than on the surface.
The left main coronary artery is associated with a higher risk for a cardiac death and usually receives a double bypass.
The presumed number of bypass grafts needed as well as the location for graft attachment is determined prior to surgery, but the final decision as to number and location is made during surgery by direct examination of the heart.
Acute renal failure due to embolism or hypoperfusion.
Stroke, secondary to embolism or hypoperfusion.
Vasoplegic syndrome, secondary to cardiopulmonary bypass and hypothermia
Pneumothorax
Hemothorax
Pericardial tamponade:
Pleural effusion
Pericarditis
Lower extremity edema, extravasation, inflammation, and ecchymoses from vein harvest.
Open heart surgery associated:
Post-operative atrial fibrillation and atrial flutter.
Anemia -secondary to blood loss, plus the anemia of inflammation.
A fall in the hemoglobin from normal preoperative levels (e.g. 15) to postoperative levels of 6 to 10 Gm are common.
Delayed healing or refracture of sternum.
Infection at incision sites;
Sepsis
Deep vein thrombosis
Anesthetic complications such as malignant hyperthermia
Keloid scarring
Chronic pain at incision sites
Chronic stress related illnesses
Late graft stenosis, particularly of saphenous vein grafts due to atherosclerosis causing recurrent angina or myocardial infarction.
With on-pump surgery, the surgeon sutures cannulae into the heart and starts cardiopulmonary bypass (CPB) by one or two
Technical approaches: either the surgeon places the aortic cross-clamp across the aorta and delivers cardioplegia with a cooled potassium mixture to stop the heart and slow its metabolism or by performing bypasses on the beating state of the heart.
One end of each vein graft is sewn on to the coronary arteries beyond the obstruction and the other end is attached to the aorta or one of its branches.
For the internal thoracic artery, the artery is severed and the proximal intact artery is sewn to the LAD beyond the obstruction.
Once the grafts, the patient is rewarmed to a normal temperature and the heart and other pressures are normal weaning off the bypass machine begins.
Chest tubes are placed in the mediastinal and pleural space to drain blood from around the heart and lungs.
The sternum is wired together and the incisions are sutured closed.
Off-pump coronary artery bypass is performed without the use of cardiopulmonary bypass with the heart-lung machine.
The avoidance of aortic manipulation through the no-touch technique,
reduces stroke and mortality compared to on-pump CABG.
Refinements of the off pump CABG have resulted in minimally invasive direct coronary artery bypass surgery, a technique of performing bypass surgery through a 5 to 10 cm incision.
Hybrid coronary revacularization, where the left internal mammary artery-to-LAD anastomosis is combined with percutaneous stents in other atherosclerotic sites, has been shown to have significant advantages compared to conventional CABG, including a decrease in the incidence of blood transfusion, and a reduced intubation time.
Typically, the left internal thoracic artery (LITA), previously referred to as left internal mammary artery or LIMA, is grafted to the left anterior descending artery and a combination of other arteries and veins is used for other coronary arteries.
The great saphenous vein from the leg is used approximately in 80% of all grafts for CABG.
The right internal thoracic mammary artery and the radial artery are frequently used as well.
The radial artery and saphenous vein graft are harvested either endoscopically, or with the open-bridging technique, employing two or three small incisions.
A cardiac stress test at five years after CABG is recommended, even in the absence of cardiac symptoms.
A medical regimen including statins, aspirin, and aerobic exercise is essential to delaying the progression of plaque formation in both the native and grafted vessels.
CABG is one of the most common procedures performed during U.S. hospital stays.
it accounted for 1.4% of all operating room procedures performed in 2011.[43] Between 2001 and 2011, however, its volume decreased by 46%, from 395,000 operating procedures performed in 2001 to 213,700 procedures in 2011.[44]
Metaanalysis show that the use of aspirin early after CABG surgery compared with controls reduced saphenous graft occlusion with an absolute reduction of 13%.
The use of dual antiplatelet therapy versus aspirin alone suggest that the outcome of saphenous vein graft failure was significantly reduced by the combination therapy at the risk of increased bleeding.
However, the risks of bleeding and associated higher mortality rate suggests that the use of dual therapy outweighs the benefits of reducing ischemic events.
The use of oral anticoagulation in most trials does not show benefit in maintaining graft patency.
Aggressive lipid-lowering reduces progression of atherosclerosis in grafts.
In a study of 1.3 million people in the US from 2011 to 2020 23% of women died or experience complications after the operation compared with 17% of men, operative mortality, was also higher women than men at 2.8% and 1.7%, respectively: 25% of patients in the group were women (Gaudino M)
In them above study women were on average two years older than men at the time of surgery, and more likely to have hypertension, diabetes, peripheral vascular disease, chronic lung disease., and more likely to have urgent unscheduled CABG surgery.
Women are older and sicker than when they have CABG surgery.