 1508
1508
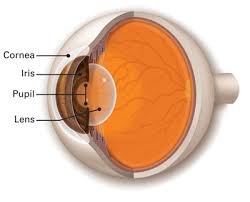
The cornea is the transparent front part of the eye that covers the iris, pupil, and anterior chamber.
The cornea, with the anterior chamber and lens, refracts light, with the cornea accounting for approximately two-thirds of the eye’s total optical power.
The refractive power of the cornea is approximately 43 dioptres.
The cornea contributes most of the eye’s focusing power, and its focus is fixed.
The cornea transmits light and provides approximately 2/3 of the eyes focusing power.
The curvature of the lens can be adjusted to depending upon the object’s distance.
The cornea has unmyelinated nerve endings sensitive to touch, temperature and chemicals.
Touching the cornea results in an involuntary reflex to close the eyelid.
The cornea does not have blood vessels, and receives nutrients via diffusion from the tear fluid through the outside surface and the aqueous humour through the inside surface, and also from neurotrophins supplied by nerve fibers that innervate it.
The cornea is required to be transparent to transmit light to the retina.
Because of injury, infection or inflammation, an area of opacity may develop which can be seen with a penlight or slit lamp.
In rare instances, this opacity is congenital.
There can be a family history of corneal growth disorders which may be progressive with age.
More commonly, misuse of contact lenses may be a precipitating factor for corneal opacity.
Corneal opacities are potentially serious and sometimes necessitates urgent treatment and corneal are the fourth leading cause of blindness.
Opacities may be keratic, that is, due to the deposition of inflammatory cells, hazy, usually from corneal edema, or they may be localized in the case of corneal ulcer or keratitis.
Corneal epithelial disruptions may be detected with fluorescein staining of the eye, and careful observation with cobalt-blue light.
Corneal epithelial disruptions would stain green, which represents some injury of the corneal epithelium.
These types of disruptions may be due to corneal inflammations or physical trauma to the cornea, such as a foreign body.
Most corneal nerve fibers are sensory in origin and are derived from the ophthalmic branch of the trigeminal nerve.
The most common causes of loss of corneal sensitivity are viral infections (herpes simplex and herpes zoster ophthalmicus), chemical burns, physical injuries, corneal surgery, neurosurgery, chronic use of topical medications, or chronic use of contact lenses.
Of the causes of loss of corneal sensitivity include systemic diseases such as diabetes mellitus, multiple sclerosis or leprosy.
The cornea has a diameter of about 11.5 mm and a thickness of 0.5-0.6 mm in the center and 0.6-0.8 mm at the periphery.
The corneal endothelium is derived from the neural crest and has an important role in corneal transparency.
Corneal endothelial cells are arrested in the G1 phase have limited proliferative ability.
Corneal endothelial cells decrease at a rate of 0.6% annually without affecting corneal transparency.
Severe damage to the corneal endothelium leads to irreversible reduction in the endothelial function, corneal edema, and loss of vision.
Has no blood supply.
Derives it’s oxygen directly through the air, as it dissolves in tears and then diffuses throughout the cornea.
It borders with the sclera by the corneal limbus.
Its soluble protein is albumin.
The human cornea has five, and possibly six, layers:
Corneal epithelium: a thin multicellular epithelial tissue layer of fast-growing and rapidly regenerated cells, that is kept moist with tears.
With any irregularity or swelling of the corneal epithelium the smoothness of the air/tear-film interface is disrupted.
The corneal epithelium is most significant component of the total refractive power of the eye, and any impairment reduces visual acuity.
The corneal epithelium is continuous with the conjunctival epithelium, and is composed of about 6 layers of cells which are continuously shedding and are regenerated by the basal layer.
Bowman’s layer, the anterior limiting membrane, is composed of collagen, laminin, nidogen, perlecan that protecting the corneal stroma.
Bowman’s layer is acellular, and is composed primarily of woven collagen fibrils that interact with and attach onto each other.
The corneal stroma is a thick, transparent middle layer.
The corneal stroma has regularly arranged collagen fibers and sparse interconnected keratocytes.
The keratocytes are the cells for general repair and maintenance of the cornea.
The corneal stroma consists of approximately 200 layers of primarily type I collagen fibrils, with each layer 1.5-2.5 μm.
Up to 90% of the corneal thickness is composed of stroma.
Descemet’s membrane, the posterior limiting membrane, is a thin acellular layer that serves as the modified basement membrane of the corneal endothelium, from which the cells are derived.
Descemet’s membrane is composed mainly of collagen type IV fibrils, less rigid than collagen type I fibrils, and is around 5-20 μm thick.
Descemet’s membrane thickness depends on the person’s age.
Corneal endothelium consists of a simple squamous or low cuboidal monolayer, approx 5 μm thick, of mitochondria-rich cells.
Corneal endothelium cells are responsible for regulating fluid and solute transport between the aqueous and corneal stromal compartments.
The corneal endothelium is bathed by aqueous humor, not by blood or lymph.
The cells of the endothelium do not regenerate, but stretch to compensate for dead cells reducing the overall cell density of the endothelium.
As the cell density reduces it can no longer maintain a proper fluid balance.
Reduced cell density results in stromal swelling due to excess fluids, and loss of transparency impairing the image formed.
The cornea is extremely innervated with sensory nerve fibers of the ophthalmic division of the trigeminal nerve by way of 70–80 long ciliary nerves and short ciliary nerves.
The density of pain receptors in the cornea is 300-600 times greater than skin and 20-40 times greater than dental pulp.
A corneal injury is very painful due to its sensory innervation.
The ciliary nerves exit the eye through holes in the sclera apart from the optic nerve.
The nerves enter the cornea via three levels; scleral, episcleral and conjunctival.
Nerve innervation involves midstromal, subepithelial/sub-basal, and epithelial tissue of the cornea.
Nerve innervation of the cornea decreases with age.
The cornea has a refractive index of 1.376, and the aqueous and vitreous humors both have a refractive index of 1.336-1.339, and they a negligible refractive effect, typically -6 diopters.
The change in refractive index between cornea and aqueous humor is relatively small compared to the change at the air–cornea interface,
The cornea may be affected by:
Corneal abrasion involving the loss of the surface epithelial layer as a result of trauma to the surface of the eye.
Corneal dystrophy in which one or more parts of the cornea lose clarity due to a buildup of cloudy material.
Corneal ulceration, an inflammatory or infective condition, involving disruption of its epithelial layer with involvement of the corneal stroma.
Corneal neovascularization caused by deprivation of oxygen from the air, results in excessive ingrowth of blood vessels from the limbal vascular plexus.
Fuchs endothelial corneal dystrophy is estimated at 4% of the US population and is the primary cause of endogenous corneal endothelial degeneration, often leading to corneal transplantation.
Fuchs endothelial corneal dystrophy is characterized by decreased endothelial cell density and formation of extracellular matrix excrescences on the posterior Descemet membrane, causing light scattering glare and visual problems.
Fuchs’ dystrophy, the process of cloudy morning vision.
Inflammation of the cornea, keratitis.
Corneal infection, infectious keratitis, can cause vision loss through corneal scarring or perforation.
Keratitis is mostly due to infection, and is estimated to account for approximately 1 million healthcare visit in the US annually.
Keratoconus, a degenerative disease, with corneal thinning and clonal changes in shape.
Surgical procedures can change the shape of the cornea to reduce the need for corrective and improve the refractive state of the eye.
Reshaping of the cornea is performed by photoablation using the excimer laser.
If the corneal stroma develops significant opacities, irregularities, or edema, it can be replaced by a transplant from a deceased person.
As there are no blood vessels in the cornea, only a few problems with rejection of the new cornea occur.
Corneal findings maya presenting sign of systemic diseases including: Wilson’s disease, gout, cystinosis, Fabry’s disease, and hyperlipoproteinemia, mucopolysaccharidosis, mucolipidosis, and amyloidosis.
Gout may be associated with fine deposits, refractile yellow crystals in the corneal epithelium and stroma.
