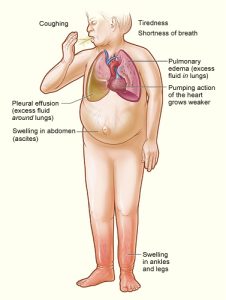
 Symptoms include shortness of breath edema and fatigue.
Symptoms include shortness of breath edema and fatigue.
The final common pathway of myocardial dysfunction in most forms of heart disease.
Cardiac arrest and arrhythmia are the major causes of death.
Affects 6-10% of adults 65 years of age and older and is increasing in prevalence.
Community prevalence of 2.5%.
Effects and estimated 26 million people worldwide.
Accounts for more than 1 million hospital admission per year.
Accounts for 1-2% of total healthcare costs in industrialized countries.
550, 000 new cases/year with 4.6 million under treatment.
There are more then 1 million hospitalizations for heart failure annually in United States, with mortality and readmission rates up to 50% within 60-90 days after discharge.
Readmission rate nearly 1 in 4 within 30 days of index discharge.
More than 60% of patients re admitted to the hospital return within the first fifteen days.
Of 30 day readmissions for CHF, 35% are related to directly to heart failure.
The annual frequency of heart transplantation is about 1% of the general population with heart failure.
In the Efficacy of Vasopressin Antagonism in Heart Failure Outcome Study with Tolvaptan (EVEREST) trial patients with no evidence of orthopnea, pedal edema, or jugular venous distention at discharge experienced a heart failure re-hospitalization rate of 26.2% and an all cause mortality rate of 19.1% during follow up at 9.9 months.
Only 50% of patients with heart failure lose more than 2 kg of fluid during hospitalizations.
Incidence and prevalence are increasing.
Annual mortality 10-11%.
At the age of 40 years, the lifetime risk is 20%.
Because the population is aging and because of advancements in medical therapy, patients with advanced disease are now much older than previous patients, and they develop more comorbidities.
Annual cost for managing heart failure is $40 billion.
CHF that has the largest number of 30 day all-cause readmissions contributing to estimated $4.3 billion in annual hospital costs.
In hospital and 60-90 day mortality for heart failure 8% and 13%, respectively.
Mortality of CHF is increased by 20% when a concomitant diagnosis of pneumonia is made.
As the population ages a shift towards a greater prevalence of heart failure with preserved left ventricular function, the stiff-heart syndrome, is occurring.
Heart with preserved systolic function presently accounts for up to two thirds of cases in patients older than the age of 70 years (Zile MR).
Historical and physical findings that support the diagnosis of CHF include orthopnea, paroxysmal nocturnal dyspnea, jugular venous distention, extra heart sounds and peripheral edema.
No single test can establish the clinical diagnosis.
Alveolar and interstitial lung infiltrates may be seen on radiographs, and cardiomegally and pleural effusions are common.
Signs and symptoms of congestion and or end organ hypoperfusion help to make the diagnosis.
The percentage of patients who acutely die from myocardial infarction has decreased nearly 30% in the last 2 decades, while the number of patients dying from congestive heart failure has doubled..
Nearly 300,000 Americana die of heart failure each year with 15-25% of these people awaiting heart transplant.
In mild heart failure the annual mortality is 5-10% and in severe cases it increases to 30-40% annually one-year survival 76%, 5-year survival 35%.
With modern medical treatments 50% of patients now live 8 years.
Mortality exceeds that of most cancers, although recent reports indicate improving prognosis.
Hospital readmission is approximately 25% within the first 6 months after hospital discharge.
More than 1 million hospitalizations for heart failure annually and more than 80% of these hospitalized patients have worsening chronic heart failure.
Of patients hospitalized heart failure patients approximately 25% to re-hospitalized with in 30 days and 30% may die within one year.
Lower income is a positive predictor for readmission risk.
Survival at 10 years 20% with initial ejection fraction of 25% and 40% with and initial ejection fraction of 35%.
Associated with myocyte hypertrophy, dysfunction and death along with increased deposition of alterations in extracellular matrix.
Patients commonly have regions of delayed myocardial activation and contraction leading to cardiac dyssynchrony.
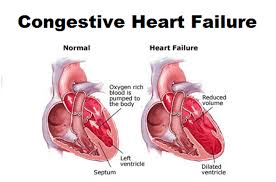
Cardiac remodeling is characterized by myocyte hypertrophy, chamber dilatation, and changes in the composition of the matrix.
Failing hearts show on microscopic evaluation a small fraction of apoptosis of cardio myocytes and many cardiac muscle cells become enlarged.
Fibrosis is evident in the myocardium of patients with CHF with proliferation of fibroblasts and altered production of extracellular matrix protein.
As a result of the above stiffness of the cardiac muscle and reduced myocardial systolic and diastolic function occur.
Cardiac remodeling leads to a fibrotic heart and becomes somewhat spherical, and loses efficiency as a pump.
An important goal is to identify and favorably intervene before terminal myocardial remodeling begins.
Angioconverting enzyme inhibitors standard therapy when CHF due to left ventricular systolic dysfunction.
About 50% of hospitalizations for heart failure are in patients that have preserved left ventricular ejection fraction, and for which there is no evidence-based treatment.
15-30% reduction in mortality with ACE inhibitors.
Poor glycemic control associated with an increased risk of CHF.
2-year survival for patients with persistent NYHA class symptoms may be only 25%.
Male sex, less education, physical inactivity, cigarette smoking, overweight, diabetes, hypertension, valvular heart disease and coronary heart disease are all independent risk factors for CHF.
Heart failure and type two diabetes are linked.
When heart failure develops in patients with type two diabetes it is complicated by markedly higher rates of mortality.
More than 60% of CHF that occurs in the U.S. population might be attributable to coronary heart disease.
Of those with coronary artery disease 90% have had a myocardial infarction.
Patients with impaired renal function have increased vulnerability to develop congestive heart failure.
In elderly roughly half of patients have normal or borderline ejection fractions.
Diastolic heart failure refers to heart failure with a normal ejection fraction.
It may be divided into three categories: one, systolic depressed function as a predominant feature, two, diastolic resulting from fibrosis and infiltrative disorders that restrict filling and cause elevated pressures, and three, a variety of conditions involving multiple features of renal and cardiovascular systems (Kass DA).
Kidney failure is very common in patients suffering from congestive heart failure, and it complicates one-third of all hospital admissions for heart failure
Approximately 50% of adults with CHF do not have left ventricular systolic dysfunction, in these patients left ventricular diastolic dysfunction exists.
Patients with preserved ejection fraction tend to be older, more likely to be female and have a history of hypertension than those patients without preserved ejection fracture.
More than 40% of patients admitted to the hospital for decompensated
heart failure have preserved systolic function ( heart failure with preserved injection fraction-HFPEF and diastolic dysfunction.
More patients will be presenting with HFPEF many of whom will be older women and will have hypertension and/or diabetes.
Patients with acute CHF and low BP associated with a poor prognosis in the short and long-term and patients with relatively high BP have lower rates of left ventricular dysfunction compared to those with low BP on admission(Gheorghiade M).
Spironolactone improves the prognosis for patients with heart failure and reduced left ventricular ejection fraction.
In patients with heart failure and preserved ejection fraction spironolactone use does not significantly reduce the incidence of death from cardiovascular causes, aborted cardiac arrest, or hospitalization for the management of heart failure (TOPCAT Investigators).
Mortality due to diastolic heart failure half the mortality rate of systolic heart failure, although not all studies have shown this result suggesting the mortality rate is equal.
The benefits of most medical therapies for heart failure is limited to those with the reduced ejection fraction, generally 40% or less.
Clinical examination cannot discriminate between systolic and diastolic heart failure, as both conditions are associated with cardiomegaly or S3 gallop.
Rales, a sign of pulmonary venous congestion, are often absent in CHF due to chronic lymphatic hypertrophy, which prevents alveolar edema despite elevated interstitial pressures (Stevenson LW).
Framingham criteria emphasize the significance of jugular venous pressure elevation, the presence of an S3 gallop and a positive hepatojugular reflex, while minimizing lower extremity edema in making the diagnosis (Mckee PA).
Patients with reduced ejection fraction have higher rates of diabetes, coronary artery disease and hyperlipidemia.
Patients with preserved ejection fraction have a higher rate of atrial fibrillation and chronic obstructive lung disease.
Prevalence of heart failure with preserved ejection fraction has increased significantly from 1987 to 2001 and such patients fare slightly better than patients with reduced ejection fraction.
While patients with preserved ejection fraction and CHF do slightly better than patients with reduced ejection fraction their survival has not improved in recent years as it has for those with reduced ejection fraction.
Patients with preserved ejection fraction have complication rates similar to patients with reduced ejection fraction, with similar rates of cardiac arrest, renal insufficiency and acute coronary artery syndrome.
Patients with preserved ejection fraction have a 30 day and 1 year mortality rate that is not significantly lower than patients with reduced ejection fraction.
It is difficult to distinguish clinically between patients with congestive heart failure with preserved ejection fraction vs. those with reduced ejection fraction and reliance on echocardiography is needed.
Among patients in sinus rhythm higher LVEF’s (left ventricular ejection fraction) associated with a linear decrease in mortality up to an LVEF of 45%.
Higher risk of adverse events with low levels of low density lipoprotein cholesterol.
In patients with CHF and left bundle branch block (LBBB) the prognosis is worse than for those without a LBBB.
In an Italian series the rate of death from any cause at one year was 16.1% for patients with LBBB and 10.5% for those without it , while the risk of sudden death at one year was 7.3% for those with LBBB and 4.9% with those without it.
With mild heart failure NYHA class I to II and on ACE inhibitors the cumulative mortality is 14.8% after 37 months.
Plasma aldosterone levels may reach up to 20 times the normal level.
Cytokines TNF and IL-6 are increased with HF and associated with worse survival.
The gold standard in diagnosing left ventricular diastolic dysfunction requires cardiac catheterization.
Elevated resting heart rate associated with cardiovascular complications and poor outcomes in different disease states, including heart failure.
Current target of heart failure treatment is to reduce heart rate and the benefits of beta-adrenergic blocking drugs are thought to be due to such a reduction.
Diuretic therapy is the mainstay of treatment for patients with CHF.
Loop diuretics which inhibit sodium-potassium-2CL transport symporter, leading to decreased sodium absorption in the ascending loop of Henle and are the most commonly used diuretics.
Beta-blockers added to standard therapy for CHF improves survival, decreases morbidity and increases well-being.
If loop diuretics are insufficient, additional diuretics that affect either the sodium chloride cotransporter such is thiazides or the renal mineralocorticoid receptor such as aldosterone antagonist are used.
Beta-blockers should be added to congestive heart failure patients only when the patient is stable.
Depression is a common comorbidity in patients with chronic heart failure, with a reported incidence of approximately 48% in this population.
Depression in patients with heart failure associated with increased mortality and hospitalization.
More common in black population.
Affects 3% of all black adults in U.S.
Anemia prevalence is below 10% among patients with mild heart failure to over 40% patients in patients with severe disease.
Anemia is associated with older age, diabetes mellitus, chronic renal impairment, more advanced heart failure, lower excercise capacity and lower quality of life.
Patients with anemia and heart failure have a lower functional capacity, impaired quality-of-life, higher rates of hospitalization and death than those patients without anemia.
Anemia helps predict rehospitalization rate and survival in chronic heart failure.
The causes of anemia in patients with heart failure is frequently unknown, but may be related to an absolute or relative deficiency, or resistance to erythropoietin.
In CHF a interaction between cardiac performance, activation of neurohormonal and inflammatory effects, renal dysfunction, adverse effects of drugs, and impaired bone marrow response contribute to the development of anemia.
Anemia in patients with congestive Cortelyou is associated with impaired renal function, inflammatory changes, and the use of renin-angiotensin system blockers.
Patient with heart failure have decreased renal perfusion, which activates the sympathetic and renin-angiotensin-aldosterone system (RAAS) and leads to the vicious cycle of water and salt retention despite the fluid overload.
The natriuretic System is impaired early and heart failure along with inappropriate levels of vasopressin together causing for the salt retention.
Evidence for recommending dietary sodium restriction in patients with heart failure is sub optimal, and there is no consensus on the optimal level of sodium intake in CHF
Scientific evidence fails to demonstrate the value of a very low sodium diet, a high sodium diet however is not in the patient’s best interest.
The above problems provide a basis for a low sodium diet in all patients with heart failure.
SODIUM-HF trial of patients with heart failure randomly assigned to dietary sodium restriction of less than 1500 mg a day or usual care without sodium restrictive diet, the incidence of death from any cause, cardiovascular related , hospitalization or cardiovascular related emergency department visit did not differ significantly between the two groups.
Correction of anemia ameliorates cardiorenal insufficiency in CHF.
Anemia of congestive heart failure associated with increased erythropoietin level in proportion to the severity of heart failure, but not to the degree of the severity of the anemia, suggesting the erythropoietin response is blunted in CHF.
In a randomized double-blind trial assigning 2270 patients with systolic heart failure and mild to moderate anemia with hemoglobin levels 9-12 g/dL to receive either darbepoetin alfa or placebo: clinical outcomes were not improved (Swedberg K et al).
Occasionally anemia in CHF may be secondary to dilution rather than to decreased red blood cell mass.
Patients with heart failure may be prone to iron deficiency secondary to depletion of iron stores or defective iron absorption and decreased availability of iron recycled by the reticuloendothelial system (Opasich C, Nanas JN).
Prevalence of iron deficiency in congestive heart failure ranges from 5-21% and may be related to malabsorption, long-term , and uremic gastritis (Anand IS).
Iron deficiency is clinically a relevant comorbidity in-up to 50% of patients with heart failure and is associated with the severity of the disease.
Iron deficiency in heart failure patients may contribute to impaired exercise capacity, quality-of-life, increased cardiac mortality, irrespective of the presence of anemia.
Iron supplementation can decrease heart failure hospitalization rate, but not all-cause mortality in patients with heart failure.
Iron therapy can increase cardiac function, exercise capacity, improve quality-of-life and prognosis in patients with heart failure.
Iron repletion can decrease serum levels of BNP and C reactive protein in patients with heart failure.
Vasopressin levels increased in CHF, and is associated with LVIV dysfunction.
Intravenous iron in patients with congestive heart failure and iron deficiency anemia improved the Minnesota Living with Heart Failure score, decreased level of CRP, BNP, and increased left ventricular ejection fraction and the distance on a 6 minute walk-test (Toblli JE).
FERRIC-HF (Ferric Iron Sucrose in Heart Failure) trial of 35 patients with iron deficiency and CHF improved global assessment score and peak oxygen uptake increased significantly in patients with anemia (Okonko DO).
Ferinject Assessment in Patients with Iron Deficiency and Chronic Heart Failure (FAIR-HF)used intravenous ferric carboxymaltose and found that in such patients, with or without anemia, symptoms are improved, functional capacity increased and quality of life improved (SD Anker).
Progresses more rapidly in black patients than in white patients.
All patients who have CHF accompanied by a low ejection fraction and who can tolerate ACE inhibitors and beta-blockers should be treated with both agents.
Framingham study has shown no improvement in the prognosis of CHF over 40 years of observation.
CA125 a marker of congestion in patients with acute heart failure.
Compared to usual care, CA 125-guided therapy is associated with marked reduction in the endpoint of one-year death or acute heart failure-related readmission in acute heart failure.
A CA 125 guided diuretic strategy improves glomerular filtration rate and other renal function parameters at 72 hours in patients with acute heart failure and renal dysfunction ( Nunez J).
Low-dose aspirin significantly reduces heart failure mortality and morbidity as demonstrated in a trial of 1400 older adults in a heart failure disease management program (Bermingham M et al).
Patients prefer the right lateral decubitus position, which leads to the highest vagal activity and the lowest sympathetic tone.
Up to 53% of patients with heart failure have intraventricular conduction delays that result in abnormal depolarization of the heart and mechanical asynchrony of the ventricles.
40% of patients with advanced heart failure may have a wide QRS complex, and those with a QRS duration of at least 140 milliseconds are at significantly increased risk for death.
Approximately one-third to half of patients have renal insufficiency with a GFR <60 mL/min per 1.73 m2 and such impairment predicts for increased mortality in patients with heart failure.
With moderate renal insufficiency ACE inhibitors improve survival, but there is little data to weigh risks and benefits to their use with more advanced renal impairment.
Survival is best able to be predicted by severity of symptoms after therapy.
In an observational study of almost 7 million Medicare patients hospitalized for congestive heart failure from 1993-2006 reductions in length of stay and in hospital mortality, and less marked reduction in 30 day mortality, aInccompanied by increases in 30 day readmission rates (Bueno H).
Approximately 14% of Medicare population has HF.
Readmission for HF ranges from 10-19% at 2 weeks to as high as 50% within 3 months.
The addition of isosorbide dinitrate and hydralazine to conventional therapy reduces relative one-year mortality by 43% in black patients.
Black patients die at a higher rate than do white patients.
ACE inhibitors less effective in blacks than in whites.
Angiotensin II receptor blocker candesartan (Atacand) added to conventional therapy results in significant reduction in cardiovascular deaths or nonfatal myocardial infarction in patients with symptomatic congestive heart failure.
Activation of the minerlcorticoid receptor by aldosterone and cortisol play a role in the pathophysiology of CHF.
Mineralcorticoid receptors are overexpressed in heart failure.
Despite the use of ACE inhibitors, ARBs and beta-blockers persistent elevations of plasma aldosterone and cortisol are present in CHF.
ACE inhibitors, ARBs and beta-blockers do not block mineralcorticoid receptors.
The Randomized Aldactone Evaluation Study (RALES) suggested that adding the mineralcorticoid-receptor antagonist spironolactone in patients with systolic heart failure and moderate to severe symptoms decreases the rate of death from any cause and risk of hospitalization for cardiovascular reasons (Pitt B et al).
In the Eplerenone Post-Acute Myocardial Infarction Heart Failure Efficacy and Survival Study (EPHESUS) the selective mineralcorticoid receptor antagonist eplerenone, added to recommended medical therapy, reduce the rates of death from any cause and hospitalization for cardiovascular reasons among patients with acute myocardial infarction complicated by left ventricular systolic dysfunction and heart failure (Pitt B et al).
In the Eplerenone in Mild Patients Hospitalization and Survival Study in Heart Failure (EMPHASIS-HF) investigated this agent added to standard care on clinical outcomes in patients with systolic heart failure and mild symptoms:Eplerenone compared with placebo reduced the risk of death and the risk of hospitalizations (Zannad F et al).
Intravenous therapy (nesiritide) for acute decompensated congestive heart failure.
Heart failure in parents associated with a 2 times higher likelihood of having left ventricular systolic dysfunction in offspring of both men and women.
Parental heart failure associated with at least a 70 percent increased in risk of heart failure in offspring, indicating the significant contribution of familial factors to the development of this process.
Parental ischemic heart failure strongly related to risk of heart failure from any cause in children.
Nonischemic heart failure not related the risk of ischemic heart failure in offspring.
In a prospective, randomized study of 308 patients with acute CHF receiving furosemide intravenously by either bolus every 12 hours or continuous infusion, and at low or high dose: no difference in patients’ global assessment of symptoms or in the change in renal function was noted by the type of adminstration (Felker GM et al).
In patients with chronic ischemic heart failure, transendocardial injection of autologous bone marrow mononuclear cells does not improve left ventricular end systolic volume, maximal oxygen consumption or reversibility on single photon emission tomography (FOCUS-CCTRN Trial).
Sodium and fluid restriction is widely used in the treatment of acute decompensation heart failure despite lack of evidence of their therapeutic benefits.
In a randomized, parallel-clinical trial the benefits of fluid and sodium restriction in patients hospitalized with acute decompensated heart failure were studied:
Fluid was restricted to 800 mL/d and sodium restricted to 800 mg per day compared to liberal fluid and sodium intake: At three days there was no effect on weight loss or clinical stability and there was significant increase in perceive thirst, concluding that sodium and water restriction in patients admitted for acute the decompensated heart failure are unnecessary (Aliti GB et al).
Clinical trials comparing fluid restricted diet versus liberal fluids in patients with heart failure have found no differences in time to clinical stabilization (Travers B et al).
A randomized controlled trial of patients stabilized after congestive heart failure failed to find benefits in fluid restriction and such treatment manifest increased thirst, dry mouth, dysgeusia, dry skin, and pruritus (Holst M et al).
Presently sodium restrictive intake recommendations for patients with acute decompensated heart failure are not specific.
In a large randomized double-blind study, the Digitalis Investigation Group trial in patients with CHF and decreased left ventricular function digoxin demonstrated reduced subsequent heart failure readmissions, all cause and cardiovascular.
Hyponatremia is common CHF and is present in 20% of patients admitted with acute heart failure and develops during decongestive treatment in additional 15 to 25%.
Hyponatremia in congestive heart failure or is associated with worse outcomes and increased mortality.
The absence of correction of hyponatremia over the course of hospitalization in patients with congestive heart failure is frequent and independently associated with an increase of approximately 50% in the odds of having the 30 day unplanned readmission or death.
Treatment options for end-stage CHF include cardiac transplant or left ventricular assist device (LVAD).therapy.
