
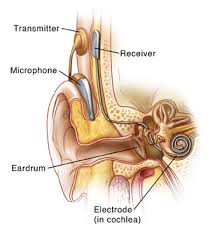
 Refers to the implant of an electrode array into the cochlea and uses a microphone near the ear to receive acoustic signals and then transmits the stimuli to the electrode, which then stimulates the cochlear nerve.
Refers to the implant of an electrode array into the cochlea and uses a microphone near the ear to receive acoustic signals and then transmits the stimuli to the electrode, which then stimulates the cochlear nerve.
A cochlear implant is an electronic device that replaces the cochlea of the inner ear.
Electrodes are typically inserted through the round window of the cochlea, into the fluid-filled scala tympani.
They stimulate the peripheral axons of the primary auditory neurons, which then send information to the brain via the auditory nerve. The cochlea is tonotopically mapped in a spiral fashion, with lower frequencies localizing at the apex of the cochlea, and high frequencies at the base of the cochlea, near the oval and round windows.
Cochlear implants acquire and process the sound and convert it into electrical energy for subsequent delivery to the auditory nerve.
Compared with hearing aids that amplify acoustic information, cochlear implants bypass the normal transduction mechanism of the peripheral auditory system and directly stimulate the auditory nerve using an electric signal.
The processor digitizes the sound and filters it into separate frequency bands that are sent to the appropriate tonotonic region in the cochlea that approximately corresponds to those frequencies.
Sound intensity is controlled by modifying current amplitude impulse duration individual electrode contacts.
Perioperative anesthetic risks are relatively low.
These devices substitute the functions performed by the eardrum and stapes while simulating the frequency analysis performed in the cochlea.
Less than 10% of adults in the US who meet the criteria for cochlear implantation receive this treatment.
A microphone on an external unit gathers the sound and processes it; the processed signal is then transferred to an implanted unit that stimulates the auditory nerve through a microelectrode array.
Due to spatial constraints, the cochlear implant may not be inserted all the way into the cochlear apex.
It provides a different kind of sound spectrum than natural hearing, but may enable the recipient to recognize speech and environmental sounds.
A period of 6 to 12 months as needed after implantation for the patient to become accustomed to hearing with the implant, and to perceive the neuroelectrical stimuli as meaningful language and sound.
Through the replacement or augmentation of damaged senses, these devices intend to improve the quality of life for those with disabilities.
Effective in children, adults with profound hearing loss.
More than half of young children with severe senorineural hearing loss are treated with cochlear implants.
Cochlear implants have allowed acquiring of spoken language development in congenitally deaf children, with remarkable success in implantations before 2–4 years of life have been reached.
There have been about 80,000 children implanted with cochlear implants worldwide.
The system transforms acoustic cues into an electrical code.
Individuals can understand speech, environmental sounds and music with varying degrees of success.
Earlier intervention with cochlear implants results in more successful language performance.
Childhood Development after Cochlear Implantation studied spoken language in children who underwent implantation prior to age 5 years: the use of cochlear implantation was associated with better spoken language learning than would have been predicted from preimplantation scores (Niparko JN).
Cochlear implantation is associated with improved comprehension, and expression of spoken language over the first 3 years of implant use.
