
 Cerebral vasculitis (angiitis) is vasculitis involving the brain and occasionally the spinal cord.
Cerebral vasculitis (angiitis) is vasculitis involving the brain and occasionally the spinal cord.
It affects all of the vessels: very small blood vessels (capillaries), medium-size blood vessels (arterioles and venules), or large blood vessels (arteries and veins).
Blood flow in a vessel with vasculitis can be reduced or stopped, and may produce a wide range of neurological symptoms, such as headache, skin rashes, malaise, joint pains, difficulty moving or coordinating part of the body, changes in sensation, and alterations in perception, thought or behavior, as well as the phenomena of a mass lesion in the brain.
Vasculitis may produce a wide range of neurological symptoms, such as headache, skin rashes, feeling very tired, joint pains, difficulty moving or coordinating part of the body, changes in sensation, and alterations in perception, thought or behavior, as well as the phenomena of a mass lesion in the brain leading to coma and herniation.
Some of its signs and symptoms may resemble multiple sclerosis.
10% of patients with cerebral vacuities have associated bleeding in the brain.
Primary angiitis/vasculitis of the central nervous system (PACNS) is said to be present if there is no underlying cause.
The fundamental mechanism of all vasculitides is autoimmune disease.
Secondary causes of cerebral vasculitis are infections, systemic auto-immune diseases such as systemic lupus erythematosus (SLE) and rheumatoid arthritis, medications and drugs (amphetamine, cocaine and heroin), some forms of cancer (lymphomas, leukemia and lung cancer) and other forms of systemic vasculitis such as granulomatosis with polyangiitis, polyarteritis nodosa or Behçet’s disease.
Cerebral vasculitis is simulated by, a number of other diseases that affect the blood vessels of the brain diffusely such as fibromuscular dysplasia and thrombotic thrombocytopenic purpura.
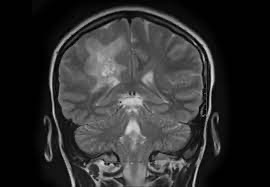
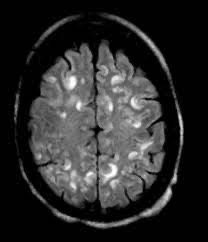
Cerebral angiography, MRI imaging, history, symptoms, physical examination, and ultimately biopsy of the brain, are often required for the diagnosis.
Laboratory; tests must be done for the diagnosis; may reveal anemia, a high white blood cell count, a high platelet count, allergic reactions, immune complexes, autoimmune antibodies and elevation of inflammatory markers.
Techniques such as conventional digital subtraction angiography (DSA) and magnetic resonance imaging (MRI) are used to find and monitor cerebral involvement.
Treatment:
Initial treatment is with many different high-dose steroids, namely glucocorticoids.
If symptoms do not improve additional immunosuppression such as cyclophosphamide are added to decrease the immune system’s attack on the body’s own tissues.
Giant cell arteritis (GCA) also known as temporal arteritis
Symptoms:Fever, general uneasiness, weight loss,inflammation of the muscles causing stiffness in the shoulders; neck; and/or upper arms, persisting headache
pain in the jaw or ear while eating
double vision, partial loss of vision or blind spots and rarely stroke.
Diagnostic criteria:
Three or more of the following.
Age 50 years or more
New developed headache
Tenderness of the superficial temporal artery
Elevated sedimentation rate, at least 50 mm/hour
Giant cell arteritis in a biopsy specimen from the temporal artery
Takayasu’s arteritis
Starts with nonspecific symptoms such as:
Localized joint pain
Fever
Fatigue
Headaches
Rashes
Weight loss
Diagnosis usually does not happen until the blockage causes deficient blood flow to the extremities or to a stroke.
Classification criteria:
Age when disease starts is under 50
Decreased brachial artery pulse
Systolic blood pressure differs by more than 10mmHg between arms
Cramping caused by exercise in the extremities
Abnormal sounds over subclavian arteries or abdominal aorta
A narrowing or blockage in the aorta, its primary branches, or large arteries as seen through a angiogram of the arteries.
Treatment of Takayasu’s arteritis:
50% of patients respond to corticosteroid therapy alone in early phases.
Methotrexate or Azathioprine are an alternative to corticosteroid immunosuppressants.
There have been studies on Mycophenolate mofetil and anti-TNF therapies.
In Takayasu’s arteritis it is vital to combine drug treatments often with low-dose aspirin or statins.
Polyarteritis nodosa
A systemic illness with fever and
general feeling of discomfort or uneasiness with cause difficult to identify
Weight loss
Arthritis
Severe inadequate blood supply to the extremities.
Ischemic stroke, hemorrhages and a progressive encephalopathy with or without seizures may occur
Diagnostic Criteria:
Three or more of the following ten criteria are required:
More than 4 kg (8.8 lb) weight loss
Lace-like purplish discoloration of the skin (livedo reticularis)
Testicular pain
Pain in a muscle or group of muscles (myalgias)
Damage to peripheral nerves
Elevation of blood pressure by more than 90 mmHg
Creatinine serum levels greater than 1,5 mg/dl
Hepatitis B or C virus antibodies
An aneurysm or occlusion as shown in a pathologic arteriography
Histology findings typical of PAN
Treatment/therapy
In PAN not associated with a hepatitis virus: prednisone and cyclophosphamide therapy. In case of emergency, plasmapheresis may be tried
In PAN associated with a hepatitis virus: combination therapy of prednisone along with a virustatic, such as lamivudine (Hepatitis B) or Ledipasvir with Sofosbuvir for hepatitis C.
Granulomatosis with polyangiitis (GPA)
Men are affected twice as often as women
Compression of structures surrounding the nose and paranasal sinuses
Diabetes insipidus
Abnormal protrusion of the eyeball(s)
Nonseptic meningitis
Affection of the lung and kidney due to destruction of the arteries and veins
Ischemic stroke, hemorrhages, or encephalopathy with possible seizures
Diagnostic Criteria:
Two or more of the following four criteria are required:
Necrotizing ulcerating inflammation of nose, sinuses, mouth or pharynx
Irregular lung infiltrates
Nephritis
Granulomatous vascular and perivascular inflammation
Treatment:
Corticosteroids
Cyclophosphamide
Azathioprine
Mycophenolate mofetil
