
 Cerebral vasculitis (angiitis) is vasculitis involving the brain and occasionally the spinal cord.
Cerebral vasculitis (angiitis) is vasculitis involving the brain and occasionally the spinal cord.
Also known as primary CNS vasculitis.
Has an annual incidence of 2.4 cases per 1 million persons and affects person of all ages and similar preferences among men and women.
Mortality ranges from 8 to 23%, with approximately 1/4 of patients having severe disability.
Mortality is associated with advanced stage, cognitive impairment at initial presentation, cerebral infarction on imaging.
Approximately 40% of patients have unfavorable outcome and 5% donnot survive long enough to be discharged from the hospital.
It affects all of the vessels: very small blood vessels (capillaries), medium-size blood vessels (arterioles and venules), or large blood vessels (arteries and veins).
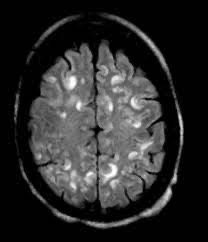
Blood flow in a vessel with vasculitis can be reduced or stopped, and may produce a wide range of neurological symptoms, such as headache, skin rashes, malaise, joint pains, difficulty moving or coordinating part of the body, changes in sensation, and alterations in perception, thought or behavior, as well as the phenomena of a mass lesion in the brain, leading to coma and herniation. The most common manifestation at initial presentation is a sudden focal neurologic deficit, suggestive of a ischemic event that includes aphasia, ataxia, and visual field defects.
Commonly patients have headaches, progressive cognitive decline and acute or subacute encephalopathy, characterized by confusion that may progress to drowsiness and coma.
Accompanying headaches are usually severe and persistent, but rarely a thunderclap headache.
Seizures, intrahemorrhage and less commonly subarachnoid hemorrhage may occur.
Spinal cord involvement with myopathy and systemic manifestation such as fever and weight loss are infrequent.
Some of its signs and symptoms may resemble multiple sclerosis.
10% of patients with cerebral vacuities have associated bleeding in the brain.
Primary angiitis/vasculitis of the central nervous system (PACNS) is said to be present if there is no underlying cause.
The fundamental mechanism of all vasculitides is autoimmune disease.
Secondary causes of cerebral vasculitis are infections, systemic auto-immune diseases such as systemic lupus erythematosus (SLE) and rheumatoid arthritis, medications and drugs (amphetamine, cocaine and heroin), some forms of cancer (lymphomas, leukemia and lung cancer) and other forms of systemic vasculitis such as granulomatosis with polyangiitis, polyarteritis nodosa or Behçet’s disease.
Cerebral vasculitis is simulated by, a number of other diseases that affect the blood vessels of the brain diffusely such as fibromuscular dysplasia and thrombotic thrombocytopenic purpura.
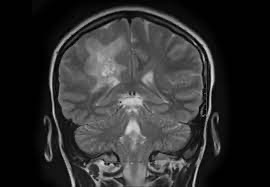
Cerebral angiography, MRI imaging, history, symptoms, physical examination, and ultimately biopsy of the brain, are often required for the diagnosis. Diagnosis is based largely on histologic evidence of vascular centered transmural inflammation with vessel wall damage.
There are three main pathological patterns include the most common granulomatous vasculitis, and lymphocytic vasculitis, with the least common necrotizing vasculitis.
Granulomatous vasculitis can be associated with amyloid beta vascular deposition beta related angiitis.
The necrotizing vasculitis is associated with cranial hemorrhage and lymphocytic vasculitis has a more benign course with less disability and lower mortality.
The primary pathophysiology is evidenced by inflammatory markers in the CSF:pro-inflammatory cytokine interleukin – 17 primarily produced by CD 4 positive T cells are elevated in the CSF.
Thr diagnostic sensitivity of brain biopsy is relatively low, with 30 to 50% of positive cases being non-diagnostic or normal, suggesting the irregular distribution vascular lesions is present.
The differential diagnosis includes reversible cerebral vasoconstriction syndrome, intracranial atherosclerosis, intravascular lymphoma, moyamoya disease and syndrome, secondary cerebral vasculitis which can occur in connective tissue diseases, systemic vasculitis, and infections.
Laboratory; tests must be done for the diagnosis; may reveal anemia, a high white blood cell count, a high platelet count, allergic reactions, immune complexes, autoimmune antibodies and elevation of inflammatory markers.
Techniques such as conventional digital subtraction angiography (DSA) and magnetic resonance imaging (MRI) are used to find and monitor cerebral involvement.
Angiographic findings suggesting vasculitis include: small, smoothwalled, segmental stenosis or multiple cerebral arteries.
Arterial occlusions are uncommon and and aneurysmal changes are rare.
Only 11.9% of patients have classic have angiographic appearance.
Digital subtraction angiography has low sensitivity of approximately 15 to 43%.
Inflammatory CSF characterized by mildly increased leukocyte count of greater than five cells per millimeter, and increased protein concentration, or both, occurs in approximately 3/4 of patients, particularly in those with small vessel vasculitis.
Treatment:
Early recognition of this disease process is important as treatment with glucocorticoids with or without cytotoxic drugs, particularly cyclophosphamide, is effective in many patients and may prevent serious outcomes.
Initial treatment is with many different high-dose steroids, namely glucocorticoids.
If symptoms do not improve additional immunosuppression such as cyclophosphamide are added to decrease the immune system’s attack on the body’s own tissues.
Additional efficacious agents include mycophenolate mofetil, rituximab, aspirin, and azathioprine.
The course of primary CNS vasculitis varies with studies suggesting induction therapy results in remission in 68 to 95% of patients.
Long term remission rates with treatment ranges from 21.5 to 66%, and flares are reported in 12 to 59% of patients.
Good neurologic functional status with low-level disability is observed in 46 to 73% of patients.
Poor therapeutic responses and long-term disability and death occur in older aged patients at diagnosis, delayed diagnostic studies, those with cognitive dysfunction at presentation, spinal cord involvement, medium to large vessel vasculitis and cerebral infarction on imaging, male gender, and lesions with gadolinium enhancement associated with the relapsing course
