 Cerebral amyloid angiopathy (CAA) is a type of cerebrovascular disorder characterized by the accumulation of amyloid beta-peptide within the leptomeninges and small/medium-sized cerebral blood vessels.
Cerebral amyloid angiopathy (CAA) is a type of cerebrovascular disorder characterized by the accumulation of amyloid beta-peptide within the leptomeninges and small/medium-sized cerebral blood vessels.
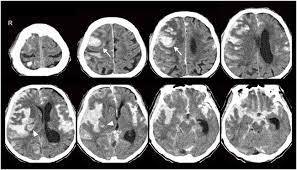
Such amyloid deposition results in fragile vessels that may manifest in lobar intracerebral hemorrhages (ICH).
CAA may also present with cognitive impairments, incidental microbleeds, hemosiderosis, inflammatory leukoencephalopathy, Alzheimer disease, or transient neurological symptoms.
CAA can induce an auto immune response.
Patient with CAA related inflammation typically have subacute encephalopathy or seizures, and sometimes focal neurologic deficits.
CAA can occur in certain familial syndromes or can sporadically.
Diagnosis is primarily made through a combination of clinical, pathological, and radiographic findings.
Neuroimaging evidence of multiple microhemorrhages or regions of cortical superficial siderosis may be seen.
CSF analysis may show mild pleocytosis and elevated protein levels, may but may also be normal.
Definitive diagnosis of CAA requires a postmortem examination of the brain.
Disease-modifying treatments are recently available.
Prognosis is dependent on CAA presenting features, with worse outcomes in patients with large hematomas and older age.
CAA is it is there second most common cause of spontaneous, intracerebral hemorrhage, characterized by deposition of misfolded beta amyloid in arteries in the cerebral cortex and leptomeninges.
It has been suggested that prion like transmissivity may occur with CAA.
Individuals receiving red blood cell transfusions from donors who later develop multiple spontaneous intracerebral hemorrhages were significantly associated with increased risk of developing spontaneous intracerebral hemorrhage compared with receiving a transfusion from donors without subsequent intracerebral hemorrhage: suggesting a transfusion transmissible agent.
Cases of presenile CAA are caused by mutations in the amyloid precursor protein (APP) gene.
Patients with APOE epsilon 2 or epsilon 4 alleles seem to be at a greater risk for cranial hemorrhages than the general population.
Cerebral amyloid angiopathy is strongly age-dependent, with the prevalence of moderate to severe CAA increasing with age.
Sporadic CAA uncommonly affects individuals younger than 60 to 65
Sporadic CAA is rare in individual in their 50s.
CAA does not appear to have a predilection for gender.
There is a possible association between hypertension and CAA.
Cerebral amyloid angiopathy is usually asymptomatic.
When symptomatic, the most common clinical manifestation of CAA is spontaneous lobar hemorrhage.
The location and the size of the hemorrhage determines the clinical deficits as extending towards the ventricles may cause hemiplegia and decreased consciousness, while smaller hemorrhage may cause more focal deficits, headaches, or seizures.
Small cerebral amyloid angio patchy hemorrhages may be asymptomatic.
The hemorrhage location reflects the distribution of the amyloid-beta peptide, and favors cortical vessels.
The hemorrhages are more likely to occur in the posterior brain, as the cerebellum commonly contains vascular amyloid accumulation.
Cognitive impairment as a presenting symptom of amyloid angiopathy:
Gradual decline – microhemorrhages, lobar lacunas, microinfarcts, ischemic leukoencephalopathy
Step-wise decline – recurrent lobar hemorrhages
Rapidly progressive decline – cerebral amyloid angiopathy-related inflammation
The Boston criteria are a combination of clinical, pathological, and radiographic criteria that are used to assess the probability of CAA.
Definitive diagnoses can only be made through a postmortem examination of the brain.
MRI is one of the most important techniques used for diagnosisGradient-echo magnetic resonance imaging (MRI) demonstrates regions of low-signal blooming artifact caused by iron depositions left by old hemorrhages.
Brain biopsies are rarely utilized in the diagnosis of CAA.
Beta-amyloid immunostain or Congo red stains are techniques that can identify deposition of amyloid beta-peptide to help support the diagnosis of CAA.
Management of CAA cerebral hemorrhage is often based on presenting symptoms.
Acute management of patients with an ICH is similar to other spontaneous ICH.
Attention to blood pressure and intracranial pressure is essential.
Factors that are associated with a worse prognosis are intraventricular hemorrhage and age greater than equal to 75.
ICH associated with CAA is frequently recurrent.
The PROGRESS trial demonstrated a risk reduction of 77% for CAA-related ICH when blood pressure was controlled.
Pulsed cyclophosphamide or glucocorticoids result in sustained clinical improvement in inflammatory CAA.
Differential Diagnosis
Nontraumatic ICH includes:
Hemorrhagic tumor
Hemorrhagic transformation of an ischemic stroke
Lobar extension of a hypertensive putaminal hemorrhage
Arteriovenous malformation (AVM)
Hypertensive microangiopathy
Hemorrhagic metastases
Multiple cavernoma syndrome
Diffuse axonal injury
Radiation-induced vasculopathy
Neurocysticercosis
The prognosis of cerebral amyloid angiopathy is determined by the location and size of the ICH.
Unfavorable outcomes are associated with larger hematoma size and the age of the patient (≥75).
Favorable ICH outcomes are associated with sparing of the ventricles and a superficial location.
Mortality ranges from 10% to 30%, with the best prognosis seen in patients with increased consciousness and smaller hematomas.
CAA has a high hemorrhage recurrence risk, compared to a hypertensive hemorrhage:recurrence rates of around 21%.
CAA is commonly associated with both transient and cognitive neurological impairment, recurrent spells of numbness, paresthesias, and weakness.
Cerebral amyloid angiopathy intracerebral hemorrhage on anticoagulant therapy has a high mortality rate.
Alzheimer disease and CAA frequently coexist.
CAA has also been found to correlate with vascular dementia.
Complications
ICH
Transient neurologic symptoms
Cortical superficial siderosis
CAA-related inflammation
Cognitive impairment
CAA can occur in certain familial syndromes or sporadically.
Diagnosis is primarily made through a combination of clinical, pathological, and radiographic findings.
Prognosis is dependent on CAA presenting features, with worse outcomes in patients with large hematomas and older age.
Earliest recognizable pathological event in Alzheimer’s disease is cerebral amyloid-beta aggregation.
Cerebral amyloid-beta may be present 20 years before the onset of dementia and Alzheimer’s disease.
Cerebral amyloid can be assessed by cerebral spinal fluid biomarkers and by positron emission tomography.
Amyloid pathology in non-demented individuals is variable, from 10-70%.
Amyloid beta pathology is associated with age, APOE genotype and the presence of cognitive impairment.
