 The caudate nucleus is one of the structures that make up the corpus striatum, which is a component of the basal ganglia in the human brain.
The caudate nucleus is one of the structures that make up the corpus striatum, which is a component of the basal ganglia in the human brain.
The caudate nucleus is associated with motor processes due to its role in Parkinson’s disease.
The caudate nucleus plays important roles in other nonmotor functions as well, including procedural learning, associative learning and inhibitory control of action, among other functions.
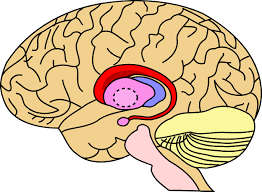
The caudate is also one of the brain structures which compose the reward system and functions as part of the cortico–basal ganglia–thalamic loop.
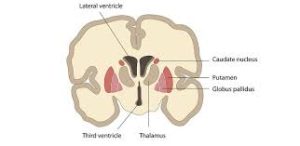
Together with the putamen, the caudate forms the dorsal striatum, and is considered a single functional structure.
The caudate nucleus it is separated by a large white matter tract, the internal capsule, so it is sometimes also referred to as two structures:
the medial dorsal striatum (the caudate) and the lateral dorsal striatum (the putamen).
The caudate nuclei are located near the center of the brain, sitting astride the thalamus.
A caudate nucleus exists within each hemisphere of the brain.
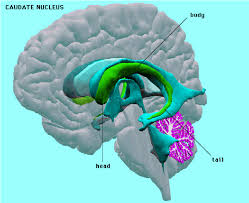
It resembles a C-shape structure with a wider head at the front, tapering to a body and a tail.
The caudate head receives its blood supply from the lenticulostriate artery.
The caudate tail receives its blood supply from the anterior choroidal artery.
The head and body of the caudate nucleus form part of the floor of the anterior horn of the lateral ventricle, and the tail forms the roof of the inferior horn of the lateral ventricle.
The caudate is innervated significantly by dopaminergic neurons that originate from the substantia nigra pars compacta (SNc).
The SNc located in the midbrain contains cell projections to the caudate and putamen, and uses the neurotransmitter dopamine.
The caudate nucleus integrates spatial information with motor behavior.
Spatial motor preparation has been linked to the caudate nucleus through event-related fMRI analysis techniques, as activity in the caudate nucleus was demonstrated to be greater during tasks featuring spatial and motoric memory demands than those that involved nonspatial tasks.
The caudate nucleus contributes to body and limb posture and the speed and accuracy of their directed movements.
The caudate nucleus inhibits the tendency to move forward without resistance.
Studies indicate a strong relationship between the caudate and frontal cortical areas associated with executive functioning.
There is a link between the caudate and goal-directed behavior
The dorsal-prefrontal cortex subcortical loop involving the caudate nucleus has been linked to deficits in working memory, specifically in schizophrenic patients.
The amygdala sends direct projections to the caudate nucleus, and both the amygdala and the caudate nucleus have direct and indirect projections to the hippocampus.
Activities associated with successful learning is concentrated to the body and tail of the caudate, while activity associated with feedback processing concentrated to the head of the caudate.
The caudate nucleus demonstrates reduced activity during non-REM sleep across all sleep stages.
This suggests the caudate nucleus has been suggested to play a role in human sleep cycles.
The caudate nucleus has been implicated in one’s responses to visual beauty.
Approach-attachment behavior and affect are also controlled by the caudate nucleus.
Patients with damage to the caudate nucleus result in loss of drive, obsessive-compulsive disorder, stimulus-bound perseverative behavior, hyperactivity, with these deficits classified as relating to approach-attachment behaviors, from approaching a target to romantic love.
The caudate is a center for language control.
Findings suggest that the left caudate is required to monitor and control lexical and language alternatives in production tasks.
The caudate nucleus is involved in degenerative diseases of the central nervous system such as Huntington disease.
In acute caudate stroke patients, 48% were found to be experiencing abulia.
Deformations of the medial caudate is correlated with verbal learning capacity for females and the number of perseverance errors on spatial and verbal fluency working memory tasks for males.
A larger caudate nucleus volume has been linked with better verbal fluency.
There is a significant reduction in activity in the left caudate nucleus during glossolalia (speaking in tongues).
Strokes can occur in the caudate nucleus, but are rare, representing only 1% of all strokes in one population of about 3,000 stroke patients.
Caudate hemorrhages account for about 7% of all intracerebral hemorrhages.
Caudate nucleus strokes can be diagnosed with CT or magnetic resonance imaging (MRI) scanning.
Caudate nucleus strokes usually involve neighboring areas like the anterior portion of the putamen, adjacent anterior limb of the internal capsule, adjacent corona radiata white matter, and globus pallidus.
About 25 to 30% of lesions are confined exclusively to the caudate.
90% of isolated caudate infarcts were unilateral and 10% are bilateral.
Small vessel disease or penetrating-branch disease is a major mechanism of caudate strokes.
Major risk factors of caudate infarcts include: hypertension, hypercholesterolemia, diabetes mellitus, previous myocardial infarct, cigarette smoking, large artery lesions, rupture of internal carotid artery aneurysms, rupture of arteriovenous malformations, cardiac embolism, and carotid artery stenosis and occlusion, non-valvular atrial fibrillation, myocardial dyskinesia, cardiac aneurysm with a mural thrombus, syphilis, Hodgkin’s lymphoma, and Moyamoya disease.
Caudate nucleus strokes frequent symptoms have included dysarthria or dysphonia (61–86%), motor weakness (40–100%), and cognitive/behavioral abnormalities (39–78%), including abulia (26–48%), agitation (29%), restlessness, hyperactivity, disinhibition (9–11%), executive dysfunction or frontal system abnormalities (26%), memory impairment, minor speech or linguistic deficits (23–50% of left-sided lesions), attention difficulties, and mood changes or depression (14–33%).
Motor weakness is often absent, minor/slight, or transient.
Abulia-decreased spontaneous verbal and motor activity and slowness, with symptoms including apathy, disinterest, flattened affect, lethargy, and lack of initiative for usual daily activities.
Cognitive and memory impairment includes poor recall, verbal amnesia (33% of left-sided lesions), and visual amnesia (right-sided lesions), among other deficits.
Caudate nucleus strokes are less commonly associated with motor disorders (20–23%), chorea (6–7%), ballism, tremor, parkinsonism (2–3%), and dystonia (9–16%), as well as more severe cognitive and behavioral problems, like psychic akinesia (12%), neglect (10% with right-sided lesions), aphasia (2–5%), and global dementia (9%,)>
Apathy, abulia, fatigue, and depression, are particularly associated with caudate strokes relative to strokes occurring in other regions.
Strokes in the caudate nucleus have also been strongly associated with post-stroke restless legs syndrome (RLS).
Other behavioral conditions, with caudate strokes include obsessive–compulsive disorder, perseverations, and mania.
Damage to the caudate nucleus usually presents with cognitive and behavioral symptoms rather than with neurological signs.
Cognitive and behavioral symptoms are more common than motor problems.
Due to the predominance of cognitive and behavioral symptoms over neurological symptoms, and frequent absence of classical stroke signs, people with caudate strokes can be misdiagnosed as having primarily psychogenic illness.
The symptoms of caudate strokes are usually more severe and persistent when they are bilateral rather than unilateral.
Caudate stroke patients have three groups based on stroke location and patterns of clinical symptoms: apathetic or abulic, with difficulties perseverating in tasks, restless, agitated, hyperactive, disinhibited, inappropriate, impulsive,distractible, and/or inattentive (ventromedial and affective disturbances (anxiety, depression, bipolar disorder) with psychotic features (hallucinations, delusions) (dorsolateral caudate, with larger lesions and more often extending into adjacent areas).
Abulia can alternate with periods of disinhibition and agitation in people with caudate strokes.
Caudate infarct symptoms are assumed to be due to interruption of neural circuits such as cortico–striatal–thalamic–cortical loops.
Caudate nucleus hemorrhages symptoms can include headache, nausea, vomiting, neck stiffness, decreased level of consciousness, hemiparesis, aphasia, neuropsychological disturbances, disorientation, aphasia, mental confusion, and gaze abnormalities, among others.
Caudate hemorrhages are due to rupture of penetrating arteries.
The prognosis of caudate strokes is good/benign, with majorities of individuals recovering and becoming independent.
Patients with caudate strokes can have residual deficits and dependency which can worsen with time.
People with caudate strokes only rarely die, and generally because of underlying heart disease or other problems rather than the stroke itself.
Lacunar strokes in general are associated with greatly increased risk of stroke recurrence, cognitive impairment and dementia, and early death.
Treatment of caudate strokes may consist of antiplatelet or anticoagulant agents and management of stroke risk factors like hypertension and diabetes mellitus to reduce the risk of additional strokes.
Disorders of diminished motivation, like apathy, abulia, and akinetic mutism, secondary to stroke and other causes, may be treated with dopaminergic agents and other medications, including psychostimulants, bupropion, atomoxetine, modafinil, dopamine agonists, levodopa, selegiline, and acetylcholinesterase inhibitors.
There is significant reduction in the caudate volume in Alzheimer’s patients when compared to the normal volunteers: it is correlated the loss of dopaminergic neurons that send axons to the caudate nucleus and the degree of dementia in Parkinson’s patients.
There is a relationship drawn between the caudate and Parkinson’s motor deficiencies, and concomitant cognitive impairments.
In Huntington’s disease, a genetic mutation occurs in the HTT gene which encodes for Htt protein.
The Htt protein interacts with over 100 other proteins, and appears to have multiple biological functions.
The behavior of this mutated protein is not is toxic to certain cell types, particularly in the brain, and is most evident in the striatum, but as the disease progresses, other areas of the brain are also more conspicuously affected.
Early symptoms are attributable to functions of the striatum and its cortical connections—namely control over movement, mood and higher cognitive function.
Caudate asymmetries related to ADHD are pronounced in the dorsal medial regions of the caudate.
The volume of white matter in the caudate nucleus has been linked with patients diagnosed with schizophrenia: patients with the disorder have smaller absolute and relative volumes of white matter in the caudate nucleus than healthy subjects.
Type I Bipolar patients had relatively higher volume of gray and white matter in the caudate nucleus and other areas associated with reward processing and decision making, compared to controls and Bipolar II subjects.
However, overall the amount of gray and white matter in Bipolar patients was lower than controls.
It is theorized that the caudate nucleus may be dysfunctional in persons with obsessive compulsive disorder (OCD), in that they may be unable to properly regulate the transmission of information regarding worrying events or ideas between the thalamus and the orbitofrontal cortex.
