 Caused by the fire, chemicals, electricity,and other elite accidents including scalding with hot water or steam.
Caused by the fire, chemicals, electricity,and other elite accidents including scalding with hot water or steam.
More then 300,000 people died each year worldwide related to the fire induced burn injuries,with many more seriously injured, disabled or disfigured.
Worldwide burn injuries are the leading cause of disability adjusted life-years lost in low and middle income countries and among the most expensive to treat traumatic injuries.
Almost all burns are preventable.
Burns are associated with intense inflammation and catabolism that predisposes patients to increase risk of infection, short and long-term organ dysfunction, and death.
Classified by how much of the skin’s thickness is involved: first degree burns (superficial) involve the top layer of the skin and are the least serious injuries, second degree, or partial thickness, burns involve deeper into the skin and cause blisters of the skin, and third-degree, full thickness, burns involving all layers of the skin, including nerves, and fourth degree burns, which extend into the muscle below the skin.
Tend to increase with lower socioeconomic status.
Up to 90% of burns occur in low-middle income countries.
In 2016 486,000 people in the US sought care for burns.
In 2016 40,000 patients were hospitalized with burns, and 30,000 of those were admitted to burn centers.
Most burns are small with 67% involving less than 10% of total body surface area.
May be associated with breathing difficulties due to hypoxia that may occur as flames can consume oxygen to the point of a low ambient oxygen level.
Dyspnea may be associated with carbon monoxide which is elevated in patients with prolonged smoke exposure.
Extensive circumferential chest and abdominal burns can lead to a compartment syndrome where patients cannot get significant breaths and may require an incision to relieve pressure.
Major surface-area burns along with smoke inhalation injury results in a greater degree of injury that can double mortality.
Smoke-inhalation injury is a result of prolonged exposure to smoke and evidence of suits or other injury below the vocal cords.
Smoke inhalation injury involves the settling of smoke particles on bronchiolar mucosa, leading to epithelial cell death, sloughing of cells, small airway obstruction, atelectasis, and increased risk of pneumonia.
The size of burns have been decreasing.
Scalding burn injuries are more common in children under the age of five years.
Flame induced burns is most common among individuals older than five years.
Most burns occur at home, and account was 75% of burn injuries.
Approximately 30% of burns occur at work.
Approximately 95% of burns are the result of an accident.
2% of burn injuries are related to abuse, and 1% are self-inflicted.
3275 deaths were reported related to burns/or smoke inhalation in 2016, with 2745 deaths resulting from the fires in residents, 310 vehicle crash related fires 220 from other causes.
It is estimated that in all low and middle income countries 180,000 people die from burns each year.
Death rates are increased with burn size, depth, smoke inhalation, and older age.
Its prevalence has a bimodal distribution based on age, with young children accounting for 24% of burns and adults 25-50 years of age accounting for 55%.
Initial management of burns concerns the airway, breathing, and circulation.
Patients with major burns may require endotracheal intubation for airway swelling.
Early intervention is considered for patients with deep burns of more than 30-40% of the total body surface area.
Lung intubation tends to be required for patients with large and deep burns, burns to the face, and those with smoke-inhalation injury.
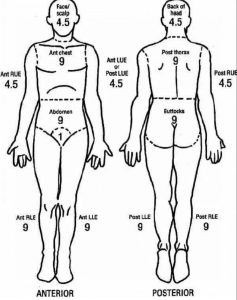
Rule of Nines estimates that each accounts for 9% of the total body-surface area, as is the head, the anterior trunk and the posterior trunk each account for 18%, as does each leg.
Most burn centers use the Lund-Browder chart to account for total body-service area variation based on age.
The extent of burns indicates the amount of fluid needed for rescuscitation.
The rate of fluid resuscitation for the first 24 hours after a burn is 2-4 mL per kilogram of body weight per percent of total body surface area that is burned, with half the volume of fluids delivered in the first eight hours.
Fluid rate management is adjusted ultimately based on urine output target of 50 mL per hour.
Excessive fluid management may lead to respiratory insufficiency, cardiac failure, and compartmental syndromes involving the trunk and extremities.
Balance isotonic crystalloids have traditionally been utilized for resuscitation, but presently most burn centers use oncotic fluids that include albumin or plasma which reduces the fluid requirements.
Hospital stay for burns is typically one day for every percent of the total body-surface area that is burned.
Management of the major burns requires three main objectives: closing the wounds, dealing with hypermetabolic response, and treating bouts of sepsis and multiple organ dysfunction that inevitably occur.
Hypermetabolism and catabolism develops in patients with burns covering more than 20% of the total body-service area and leads to muscle wasting and unless appropriately and successfully treated, death from multiple organ failure.
To reduce metabolic stress, removing burn tissue and covering the exposed area with skin or other barrier is required.
Patients with hypermetabolic response have elevated core temperatures.
Minimizing pain, infection and sepsis also reduce metabolic demand.
The use of beta blockers to reduce catecholamine effects may be beneficial.
Nutritional support is required with patients with major burns to keep up with high metabolic requirements.
Enteral feedings are started as soon as possible to maintain nutrition.
Proteins are administered at a rate of 1 1/2 -2 grams per kilogram per day.
Increasing muscle mass by promoting early mobility and exercise is advocated.
Because skin, the primary barrier to microbial invasion is lost with a burn, sepsis is a major risk factor with any large burn.
Sepsis risk persists as long as skin wounds remain open.
Prophylactic antibiotics are ineffective in preventing infection, but increases the risk of resistant organisms.
Burns lead to the persistent exposure to microbial agents, along with a hypermetabolic response including persistent elevated temperatures, and tachycardia.
All patients with large surface area burns have the systemic inflammatory response syndrome.
Frequent necessity of using central lines, mechanical ventilators, and urinary catheters increase the risk of infections in patients with serious burns.
Signs of sepsis related to burn injuries include: thrombocytopenia, feeding a tolerance, decreased urine output, acidosis, and respiratory insufficiency.
Aggressive antibiotic management with broad-spectrum aging is required.
The depth of burn injury suggests the type of care required.
A first-degree burn does not penetrate the epidermis and the skin barrier remains intact.
The burn may appear dry and red.
Minimal treatment for first- degree burns are analgesia and a moisturizer.
Healing of first-degree burns is usually rapid.
Second-degree, or partial-thickness burns penetrate into but not through the dermis.
Second-degree burns are associated with the loss of the epidermal barrier and the wound forms a blister and if uncovered weeps interstitial fluid.
With the second-degree burns the dermal plexus of blood vessels and nerves remains intact, so the wound blanches with pressure and the pain is severe.
A second-degree burn heals by re-epithelization with a basal cells migrating across viable wound bed.
Basal cells are stimulated by local growth factors and wound proteins.
Keratinocytes migrate faster in a moist environment than if the wound is dry.
The limit of wound migration is only one-2 cm, but in superficial wounds the keratinocytes in the remnant hair follicles and other skin adnexa migrate onto the surface to re-epithelialize the wound.
In elderly patients with fewer adnexal hair follicles reepitheliation is impaired.
Skin in older individuals is thinner and the consequences of a burn is greater.
As 2nd degree burn becomes deeper fewer adnexal skin tissues remain, the deeper burns require more time to heal.
When a wound requires more than 2-3 weeks to re-epithelialize there is a high chance of developing a hypertrophic scar.
Wounds that require 2-3 weeks to heal are considered for excision and skin grafting to reduce the chances of hypertrophic scar.
Re-epithelization of a partial thickness wound should be washed with soap and water, loose skin and blisters should be debrided and a topical ointment applied to maintain a moist environment.
Topical antibiotic ointment use dressings should be changed once or twice a day.
Topical ointments can be used on small wounds, but, such agents should be discontinued within a week since they invariably cause a rash.
Silver sulfadiazine impairs re-epithelization and is avoided for superficial wounds.
