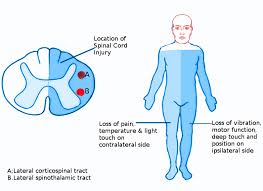
 Brown-Séquard syndrome is caused by damage to one half of the spinal cord, resulting in paralysis and loss of proprioception on the same side as the injury or lesion, and loss of pain and temperature sensation on the opposite side as the lesion.
Brown-Séquard syndrome is caused by damage to one half of the spinal cord, resulting in paralysis and loss of proprioception on the same side as the injury or lesion, and loss of pain and temperature sensation on the opposite side as the lesion.
Brown-Sequard syndrome is a result from damage to one half of the spinal cord that carries sensory and motor information between the brain and the rest of the body.
The syndrome is characterized by a combination of weakness, paralysis, or loss of sensation on one side of the body, along with a different set of symptoms on the opposite side of the body.
The spinal cord contains tracts of nerve fibers that cross over from one side of the body to the other at different levels, so damage to one side of the spinal cord affects the transmission of signals on the opposite side.
The specific symptoms of Brown-Sequard syndrome depend on the location of the spinal cord injury.
Common features include:
Weakness or paralysis on one side of the body
Sensory loss or decreased sensation on the opposite side of the body.
Loss of pain and temperature sensation on the side of the body affected by paralysis
Retained sense of position, touch, and vibration on the side of the body affected by paralysis
BSS commonly results from a spinal cord injury due to penetrating trauma, such as a knife wound or gunshot wound, although it can also occur due to other causes such as a spinal tumor or infection.
Treatment typically involves supportive care and rehabilitation to improve function and overall quality of life.
BSS may be caused by injury to the spinal cord resulting from a spinal cord tumor, trauma, ischemia or infectious or inflammatory diseases such as tuberculosis, or multiple sclerosis.
The most common cause is penetrating trauma such as a gunshot wound or stab wound to the spinal cord.
Decompression sickness may also be a cause of Brown-Séquard syndrome.
The presentation of BSS can be progressive and incomplete.
It can advance from a typical Brown-Séquard syndrome to complete paralysis.
It BSS is not always permanent and progression or resolution depends on the severity of the original spinal cord injury and the underlying pathology that caused it in the first place.
The hemisection of the cord results in a lesion of each of the three main neural systems:
the principal upper motor neuron pathway of the corticospinal tract
one or both dorsal columns
the spinothalamic tract
As a result of the injury to these three main brain pathways the patient will present with three lesions:
The corticospinal lesion produces spastic paralysis on the same side of the body below the level of the lesion.
At the level of the lesion, there will be flaccid paralysis of the muscles supplied by the nerve of that level.
The lesion to fasciculus gracilis or fasciculus cuneatus (dorsal column) results in ipsilateral loss of vibration and proprioception as well as loss of all sensation of fine touch.
The loss of the spinothalamic tract leads to pain and temperature sensation being lost from the contralateral side beginning one or two segments below the lesion.
In addition, if the lesion occurs above T1 of the spinal cord it will produce ipsilateral Horner’s syndrome with involvement of the oculosympathetic pathway.
Diagnosis:
Magnetic resonance imaging (MRI) is the imaging of choice in spinal cord lesions.
It is diagnosed by finding motor (muscle) paralysis on the same (ipsilateral) side as the lesion and deficits in pain and temperature sensation on the opposite (contralateral) side.
This is called ipsilateral hemiplegia and contralateral pain and temperature sensation deficits.
The loss of sensation on the opposite side of the lesion is because the nerve fibers of the spinothalamic tract (which carry information about pain and temperature) crossover once they meet the spinal cord from the peripheries.
Crude touch, pain and temperature fibers are carried in the spinothalamic tract, which decussate at the level of the spinal cord.
Therefore, a hemi-section lesion to the spinal cord will demonstrate loss of these modalities on the contralateral side of the lesion, while preserving them on the ipsilateral side.
Upon touching this side, the patient will not be able to localize where they were touched, only that they were touched,
because fine touch fibers are carried in the dorsal column-medial lemniscus pathway.
The fibers in this pathway decussate at the level of the medulla.
Therefore, a hemi-section lesion of the spinal cord will demonstrate loss of fine touch on ipsilateral side and preserved on the contralateral side and crude touch, the destruction of the decussated spinothalamic fibers from the contralateral side on the contralateral side.
Pure Brown-Séquard syndrome is associated with the following:
Interruption of the lateral corticospinal tracts:
Ipsilateral spastic paralysis below the level of the lesion
Babinski sign ipsilateral to lesion
Abnormal reflexes and Babinski sign may not be present in acute injury
Interruption of posterior white column:
Ipsilateral loss of tactile discrimination, vibratory, and position sensation below the level of the lesion
Interruption of lateral spinothalamic tracts:
Contralateral loss of pain and temperature sensation.
This usually occurs 2–3 segments below the level of the lesion.
Treatment:
Treatment is directed at the pathology causing the paralysis.
Brown-Séquard syndrome is rare as the trauma would have to be something that damaged the nerve fibres on just one half of the spinal cord.
