 Bacterial meningitis causes approximately 318,000 deaths annually worldwide, and an estimated 20,383 years of life lost.
Bacterial meningitis causes approximately 318,000 deaths annually worldwide, and an estimated 20,383 years of life lost.
Incidence of community acquired bacterial meningitis is about 2.5 to 3.5 cases per 100,000 population, this represents a 55% reduction in cases less than 10 years ago.
The incidence ranges from approximately 0.9 per 100,000 individuals per year in high income countries to approximately 10 to 80 per hundred thousand individuals per year in low income and middle income countries.
With use of highly effective bacterial conjugate vaccines against Haemophilus influenzae type b and Streptococcus pneumoniae incidence in children has decreased significantly.
Annual incidence 4-6 cases per 100,000 adults.
The classic triad of fever, stiff neck, and change in mental status occurs only in about 41% of patients with acute bacterial meningitis.
The classic presentation of bacterial meningitis is more common in patients older than 60 years.
Most common presenting symptoms are headache, fever, stiff neck, altered mental status, and nausea.
Occasionally patients may present with aphasia or hemiparesis or monoparesis, coma, cranial nerve palsy, and rash.
A concomitant infection typically involves the sinuses, otitis, pneumonia, and endocarditis.
Mortality rates in adults and neonates with bacterial meningitis range from 6 to 54%.
In neonate Streptococcus agalactiae, E. coli, and Listeria monocytogenes these are the most common causes of bacterial meningitis.
Group B streptococcus can be early onset between birth and six days of age, or late onset, between seven and 89 days of age and can be prevented with non-vaccine interventions.
Up to 40% of pregnant patients have their rectum or vaginal tract colonized with Group B streptococci and is the leading cause of neonatal exposure.
The CDC recommends performing rectal and vaginal cultures at approximately 36-37 weeks of pregnancy to detect Group B streptococci colonization.
Patients with colonization should receive intravenous penicillin G during labor and delivery.
Intravenous penicillin does not preventlate onset Group B meningitis.
Mortality varies from 10% in higher income countries to 58% in low income countries.
Neurological sequelae of hemiparesis, cranial neuropathy, hearing loss and memory impairment vary from 9.4% in Europe to 25% in Africa.
Bacterial meningitis accounts for approximately 13% of all cases of meningitis and encephalitis in the US.
In the 1970s-80s 80% of cases of bacterial meningitis were due to Haemophilus influenzae, Streptococcus pneumoniae, Neisseria meningitidis, group B. Streptococcus and Listeria monocytogenes.
Between 1986 and 1995 the incidence of bacterial meningitis from the five agents above declined by 55% due to the H. influenzae type b conjugate vaccine for infants introduced in the United States in 1990.
Since the introduction of the heptavelent protein polysaccharide pneumococcal conjugate vaccine (PCV 7) in 2000, invasive pneumococcal disease decreased by 75% among children under the age of five and by 31% among adults 65 years or older.
Because of the success of pneumococcal and Hib vaccines in reducing rates of meningitis in children, the burden of meningeal infections has been increasingly borne by older adults.
Highest incidence is in infants less than 6 months of age.
Streptococcus pneumonia and Neisseria meningitidis responsible for 80% of cases in adults.
Incidence of bacterial meningitis caused by N. meningitidis infection is 0.6 cases per 100,000 population in the U.S.
Caused by N. meningitidis most common cause of bacterial meningitis between ages 2 and 18 years.
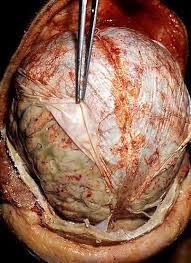
Leads to brain damage caused by inflammation, infarction or seizures was neuronal necrosis, and survivors of childhood bacterial meningitis are at risk for hearing loss, seizures, motor deficits, and cognitive impairments , and learning disabilities.
Case fatality rates and serious complications from meningitis caused by S pneumoniae infection reported to be as high as 40%.
Despite that adjunctive dexamethasone benefits adults with pneumococcal meningitis, the case fatality for bacterial meningitis remains 20%.
The incidence of pediatric bacterial meningitis in infants under 2 months of age, the group at greatest risk, has not decreased, with the major cause Group B streptococci.
In infants under 2 months Group B streptococcal meningitis manifests as late onset disease 7 days or more following birth.
Intrapartum antibiotic prophylaxis has significantly reduced the risk of early onset meningitis, but has not changed th risk of late-onset disease.
S pneumonia the most common cause of meningitis in adults.
Mortality rates caused by N meningitidis 5-10% and from H influenzae type b 3-6%.
Inflammatory response contributes to neuronal injury.
Classic triad of headache, fever and neck stiffness seen in about 44% of patients.
Approximately 95% of patients present with at least two of the following four symptoms: headache, fever, neck stiffness, and altered mental status.
Almost all patients have 2 of 4 symptoms of fever, headache, stiff neck or altered mental status with a Glasgow Coma score of less than 14.
Clinical features cannot reliably distinguish between ABM and other important infectious and non-infectious aetiologies.
Lumbar puncture (LP) and cerebrospinal fluid analysis, biochemistry and culture are the mainstay of diagnosis, but molecular techniques are increasingly useful.
There is increasing recognition that current antibiotic regimens and adjunctive therapies alone are insufficient to reduce the mortality and morbidity associated with ABM.
Up to 30% have seizures.
Patients with bacterial meningitis are usually ill in appearance and present soon after the onset of symptoms.
Components of bacterial meningitis score include: positive cerebrospinal fluid Gram stain, absolute CSF neutrophil count ≥1000 cells /microL,CSF protein ≥80 mg/dL, peripheral blood absolute neutrophil count ≥ 10,000 cells /microL, low CSF glucose, history of seizures before or at the time of presentation.
If a patient lacks all of the criteria of the bacterial meningitis score they are at very low risk for bacterial meningitis.
In the present era of use of Haemophilus influenzae type b and pneumococcal vaccines bacterial meningitis has become an uncommon disease in children and the majority of children with CSF pleocytosis have aseptic meningitis.
Most common long-term complication is sensorineural hearing loss, which occurs in about 10% of survivors.
Hemiparesis occurs in about 13% of patients.
Fever is the most sensitive of signs of meningitis and occurs in majority if cases.
Normal mental status helps exclude meningitis in low-risk patients.
Kernig and Brudzinski signs have low sensitivity but high specificity.
Eliciting or worsening headache with jolt accentuation improves yield in diagnosis.
Lumbar puncture necessary in any patient suspected of diagnosis.
CSF Gram stain sensitivity in community acquired bacterial meningitis ranges between 60 and 90%, and varies by concentration of the bacteria in CSF, type of pathogen, and by receipt of previous antibiotic therapy.
There is a risk of brain herniation as a complication of lumbar puncture.
Meta-analysis of randomized, controlled studies of the utilization of corticosteroids for bacterial meningitis between 1996 and 2001 concluded that such agents reduced the death rate and neurologic sequelae, and hearing loss in children (van de Beek).
In a study from a European group of 300 patients revealed that the use of dexamethasone resulted in fewer deaths and less disability compared with a placebo group (de Gans).
Studies have also revealed that dexamethasone use is beneficial in some adolescents and adults with bacterially confirmed disease.
Induced therapeutic hypothermia in severe bacterial meningitis utilized in a randomized clinical trial did not improve outcome in patients, and may even be harmful (Mourvillier B et al).
