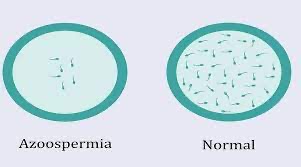
It is associated with male infertility.
Azoospermia affects about 1% of the male population.
It may be seen in up to 20% of cases of male infertility.
It is the intended result of a successful vasectomy.
There are three types of azoospermia.
Many conditions listed may also cause various degrees of oligospermia rather than azoospermia.
Pretesticular and
Testicular azoospermia are known as non-obstructive azoospermia
Post-testicular azoospermia is considered obstructive.
Pretesticular azoospermia is characterized by inadequate stimulation of otherwise normal testicles and genital tract: follicle-stimulating hormone (FSH) levels are low (hypogonadotropic) commensurate with inadequate stimulation of the testes to produce sperm.
Pretesticular azoospermia seen with hypopituitarism, hyperprolactinemia, and exogenous FSH suppression by testosterone, and chemotherapy may suppress spermatogenesis.
Pretesticular azoospermia is seen in about 2% of azoospermia, and is a kind of non-obstructive azoospermia.
Testicular azoospermia means the testes are abnormal, atrophic, or absent, and sperm production severely disturbed to absent.
FSH levels tend to be elevated as the feedback loop is interrupted by a lack of feedback inhibition on FSH.
The condition is seen in 49–93% of men with azoospermia.
Testicular failure includes absence of production and low production and maturation arrest during the process of spermatogenesis.
Causes for testicular failure include;
congenital issues such as in genetic conditions (Klinefelter syndrome), some cases of cryptorchidism or Sertoli cell-only syndrome as well as acquired conditions by infection, surgery, trauma, cancer, and radiation.
Mast cells releasing inflammatory mediators appear to directly suppress sperm motility.
Testicular azoospermia is a type of non-obstructive azoospermia.
Men with unexplained hypergonadotropic azoospermia need to undergo a chromosomal evaluation.
Post-testicular azoospermia, occurs when sperm are produced but not ejaculated, a condition that affects 7–51% of azoospermic men,
The main cause is a physical obstruction of the post-testicular genital tracts, and
the most common reason is a vasectomy done to induce contraceptive sterility.
Other causes of obstructions can be congenital or acquired, such as ejaculatory duct obstruction by infection.
Ejaculatory disorders include retrograde ejaculation and anejaculation; in these conditions sperm are produced but not expelled.
Oligospermia and azoospermia are significantly associated with being obese.
The frequency of chromosomal abnormalities is inversely proportional to the semen count, thus males with azoospermia are at risk to have a 10–20% incidence of abnormalities on karyotyping versus about <1 % in the fertile male population.
Pretesticular azoospermia may be caused by congential hypopituitarism, Kallmann syndrome, Prader-Willi syndrome and other genetic conditions that lead to GnRH or gonadotropin deficiency.
Testicular azoospermia is seen in Klinefelter syndrome (XXY) and the XX male syndrome.
About 13% of men with azoospermia have a defective spermatogenesis that is linked to defects of the Y chromosome.
Defects of the Y chromosome likely to be de novo micro-deletions..
Y chromosome defects usually the long arm of the chromosome.
A section of the long arm of the Y chromosome has been termed Azoospermia Factor (AZF):
at Yq11 and subdivided into AZFa, AZFb, AZFc and possibly others.
Defects in this area can lead to oligospermia or azoospermia.
Spermatogenesis is defective with gene defects for the androgen receptor.
Post-testicular azoospermia can be seen with certain point mutations in the cystic fibrosis transmembrane conductance regulator (CFTR) gene.
The CFTR gene is commonly associated with congenital vas deferens abnormalities.
BRD7, is a transcription regulatory protein, that is normally highly expressed in the testis.
Its absence or reduced expression is observed in the testes of azoospermia patients exhibiting spermatogenesis arrest.
A common single nucleotide polymorphism in BRCA2 is associated with idiopathic male infertility with azoospermia.
Single nucleotide polymorphisms in genes TEX11 and MLH3 are associated with male infertility involving azoospermy or oligospermia.
Azoospermia is usually detected in the course of an infertility investigation: two semen analysis evaluations done at separate occasions shows no sperm under the microscope.
Evaluation of azoospermia:
history, a physical examination including a thorough evaluation of the scrotum and testes, laboratory tests, and possibly imaging.
History includes the general health, sexual health, past fertility, libido, sexual activity, and past exposure drugs.
Medical agent exposures like hormone/steroid therapy, antibiotics, 5-ASA inhibitors, alpha-blockers, 5 alpha-reductase inhibitors, chemotherapeutic agents, pesticides, recreational drugs, and alcohol should be noted.
History of heat exposure of the testes is warranted as is a history of surgical procedures of the genital system, and family history needs to be assessed to look for genetic abnormalities.
Congenital absence of the vas deferens may be detectable on physical examination and can be confirmed by a transrectal ultrasound (TRUS).
Transrectal ultrasound can identify azoospermia caused by obstruction, or anomalies related to obstruction of the ejaculatory duct, such as abnormalities within the duct itself, a median cyst of the prostate or an impairment of the seminal vesicles to become enlarged or emptied.
Retrograde ejaculation can be diagnosed by examining a post-ejaculatory urine for presence of sperm.
Low levels of LH and FSH with low or normal testosterone levels are indicative of pretesticular problems, while high levels of gonadotropins indicate testicular problems.
The differentiation between obstructive versus non-obstructive azoospermia may require a testicular biopsy.
In azoospermic men with a normal ejaculate volume, FSH serum level greater than two times the upper limit of the normal range is reliably diagnostic of dysfunctional spermatogenesis.
Serum inhibin-B weakly indicates presence of sperm cells in the testes.
Genetic evaluation is done for men with azoospermia as a result of primary hypopituitarism.
Azoospermic men with testicular failure are advised to undergo karyotype and Y-micro-deletion testing.
Treatment:
Pre- and post-testicular azoospermia are frequently correctible, while testicular azoospermia is usually permanent.
IVF with ICSI which allows successful fertilization even with immature sperm or sperm obtained directly from testicular tissue.
IVF-ICSI allows for pregnancy in couples where the man has irreversible testicular azoospermia as long as it is possible to recover sperm material from the testes.
Thus men with non-mosaic Klinefelter’s syndrome have fathered children using IVF-ICSI.
Pregnancies have been achieved in situations where azoospermia was associated with cryptorchism and sperm where obtained by testicular sperm extraction.
In men with post-testicular azoospermia: for obstructive azoospermia, IVF-ICSI or surgery can be used and individual factors are considered for the choice of treatment.
Medication may be helpful for retrograde ejaculation.
