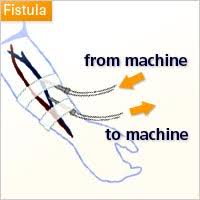
Approximately 90% of patients undergoing dialysis are treated with hemodialysis and they require vascular access to establish a connection between their circulation and the hemodialysis machine.
An arterovenous access includes any conduit created involving a direct or indirect anastomosis between an anrtery and vein for providing hemodialysis.
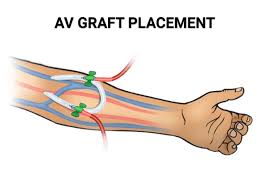
AV access refers to all to a autogenous AV fistula that is created by direct connection between an artery and a vein in which the developed outflow vein is accessed for hemodialysis with needles or AV graft, in which non-autologous material is placed between the artery and vein, which is accessed for hemodialysis.
AV access creation is typically performed under local or regional anesthesia with conscious sedation.
AV access creation is usually an outpatient procedure.
AV access can also be established with percutaneous endovascular techniques that did not require open surgery, incisions, or suture material.
Have a short life span and are prone to recurrent stenosis and thrombosis, requiring multiple procedures to maintain their patency.
AV graphs cannot be used until after 2 to 4 weeks from creation to allow proper incorporation of a graft material in the surrounding tissue and reduce the likelihood of hematoma formation with cannulation; earlier graft materials are avaluable to be used within 24 to 72 hours.
AV fistulas require approximately four months after creation before they can be used, allowing it to sustain repeated trauma of needle cannulation.
AV fistulas have a two-year cumulative patency of 63% and for AV grafts is 60%.
AV fistula is preferable AV grafts as it is associated with a fewer long-term vascular events, such as thrombosis and fewer interventions to maintaining functional patency.
Hypoalbuminemia a strong predictor of early graft intervention.
Typically made by using a synthetic tube connecting the artery and vein.
More easily cannulated than fistulas and can be use for hemodialysis sooner after surgery than fistulas.
Stenosis is the most common cause (up to 90%) that limits flow within the AV access circuit and leads to thrombosis and loss of AV access.
Neointimal hyperplasia caused by AV access flow related wall sheer stress, surgical trauma, or both and is the ultimate pathological lesion that impairs flow: the use of medication’s to prevent flow related AV access dysfunction remains unresolved.
Pe\rcutaneous balloon angioplasty is recommended for flow related AV access dysfunction and has a post intervention patency rate of 23 to 63% at six months.
In a study of 649 randomized patients to receive this agent plus aspirin or placebo in patients undergoing hemodialysis the incidence of patency at 1 year was 23% in the placebo group and 28% in a Dipyridamole-aspirin group, and the treated group had a prolonged duration of primary unassisted patency: the incidence of graft failure, death and serious events did not differ in the two groups (Dixon B.S.).
In the above study over three fourths of patients required intervention to maintain patency or to treat another access complication within the first year after graft placement (Dixon B.S.)
Patients should be monitored for the presence of a palpable pulse or thrill, or auscultated bruit and should undergo immediate intervention if there’s any chance of an AV access salvage.
Physical exam has an 82 to 100% sensitivity and a 67 to 88% specificity to detect inflow stenosis and a 70 to 97% sensitivity and 67 to 93% specificity to detect outflow stenosis.
The percentage of patient to undergo repeat intervention within six months is estimated to be approximately 50%.
Arteriovenous dialysis grafts have a thrombosis in more than 50% of cases within one year after placement, necessitating a salvage procedure in more than 75%of cases.
Arteriovenous graft thrombosis usually occurs at the venous anastomosis in proximity to a stenotic lesion that has resulted from aggressive neo-intimal hyperplasia.
The Dept. of Veterans Affairs Cooperative trial of aspirin plus clopidogrel in patients undergoing hemodialysis, who had established grafts was terminated early because of increased risk of bleeding, and the study failed to show a benefit of the drug compared to placebo for the prevention of thrombosis (Kaufman JS).
In a study of low dose warfarin in patients with an arteriovenous graft there was no reduction in the risk of thrombosis, but there was an increase risk of bleeding (Crowther MA).
Currently, treatment to maintain patency of such graft is the use of angioplasty to treat stenosis and thrombosis after it occurs.
Drug-coated balloon angioplasty is superior to standard angioplasty for the treatment of stenotic lesions in dysfunctional hemodialysis arteriovenous fistulas. (Lookstein RA).
Stent graphs covering slash encasing stents can be used to bypass stenoses.
Arterial venous access thrombosis, is 2 to 3 times more common with AV grafts versus AV fistulas.
AV access can result in hemodynamic changes with decreased perfusion of distal tissues, typically the hand.
This steal syndrome can occur in 1 to 8% of patients with AV access, and can cause both acute and chronic ischemia with finger numbness, skin mottling, rest pain, and tissue loss that can lead to amputation.
Arteriovenous fistulae and arteriovenous grafts can develop pseudoaneurysms, which are areas of focal degeneration contained by surrounding soft tissue typically caused by repeated cannulation in the same area.
Such abnormalities can compromise dialysis efficiency, limit access to cannulation sites, and result in hemorrhage due to breakdown of the overlying skin.
Arteriovenous access hemorrhage is a medical emergency that can be fatal in less than one percent of cases.
The increased cardiac output that occurs with arterovenous access can cause high output cardiac failure, and pulmonary hypertension.
25% of cases of high output heart failure are attributed to arterial venous access.
