 Angioplasty is commonly used to describe the inflation of a balloon within the coronary artery to crush the plaque into the walls of the artery.
Angioplasty is commonly used to describe the inflation of a balloon within the coronary artery to crush the plaque into the walls of the artery.
Angioplasty, is also known as balloon angioplasty is a minimally invasive endovascular procedure used to widen narrowed or obstructed arteries or veins, typically to treat arterial atherosclerosis.
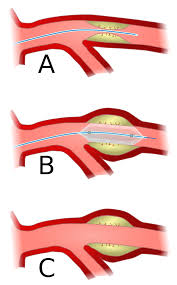
A deflated balloon attached to a balloon catheter is passed over a guide-wire into the narrowed vessel and then inflated to a fixed size.
The balloon forces expands the blood vessel and the surrounding muscular wall, allowing an improved blood flow.
The balloon is then deflated and withdrawn.
A coronary angioplasty is a therapeutic procedure to treat the stenotic coronary arteries of the heart found in coronary heart disease.
To ensure the vessel remains open a stent may be inserted at the time of ballooning.
An inverse relationship between mortality and the annual number of angioplasty procedures performed in a hospital.
Hospitals that performed a large number of primary angioplasty procedures were more likely to use aspirin, B-blockers and heparin in the first 24 hours of an myocardial infarction.
A percutaneous coronary intervention (PCI), or coronary angioplasty with stenting, is a non-surgical procedure used to improve the blood flow to the heart.
Coronary angioplasty is indicated for coronary artery disease such as unstable angina, NSTEMI, STEMI and spontaneous coronary artery perforation.
PCI for stable coronary disease has been shown to significantly relieve symptoms such as angina, or chest pain, thereby improving functional limitations and quality of life.
Renal artery stenosis is associated with hypertension and loss of renal function.
Atherosclerotic obstruction of the renal artery can be treated with angioplasty with or without stenting of the renal artery.
Carotid artery stenosis can be treated with angioplasty and carotid stenting for patients at high risk for undergoing carotid endarterectomy.
Although carotid endarterectomy is typically preferred over carotid artery stenting, stenting is indicated in select patients with radiation-induced stenosis or a carotid lesion not suitable for surgery.
Angioplasty is used to treat venous stenosis affecting hemodialysis access, with drug-coated balloon angioplasty proving to have better 6 month and 12 month patency than conventional balloon angioplasty.
Angioplasty is occasionally used to treat residual subclavian vein stenosis following thoracic outlet decompression surgery for thoracic outlet syndrome.
There is a weak recommendation for deep venous stenting to treat obstructive chronic venous disease.
Angioplasty requires an access vessel, typically the femoral or radial artery or femoral vein, to permit access to the vascular system for the wires and catheters used.
If no access vessel of sufficient size and quality is available, angioplasty is contraindicated.
A small vessel diameter, the presence of posterior calcification, occlusion, hematoma, or an earlier placement of a bypass origin, may make access to the vascular system too difficult.
Percutaneous transluminal coronary angioplasty (PTCA) is contraindicated in patients with left main coronary artery disease, due to the risk of spasm of the left main coronary artery during the procedure.
Also, PTCA is not recommended if there is less than 70% stenosis of the coronary arteries, as the stenosis it is not deemed to be hemodynamically significant below this level.
Access to the vascular system is typically gained percutaneously.
An introducer sheath is inserted into the blood vessel via the Seldinger technique.
In realtime fluoroscopic guidance uses magnetic resonance or X-ray fluoroscopy and radiopaque contrast dye to guide angled wires and catheters to the region of the body to be treated.
To treat a narrowing in a blood vessel, a wire is passed through the stenosis in the vessel and a balloon on a catheter is passed over the wire and into the desired position.
The balloon is inflated using water mixed with contrast dye to 75 to 500 times normal blood pressure, with most coronary angioplasties requiring less than 10 atmospheres.
A stent may or may not also be placed.
At the conclusion of the procedure, the balloons, wires and catheters are removed and the vessel puncture site is treated either with direct pressure or a vascular closure device.
Transradial artery access (TRA) and transfemoral artery access (TFA) are two techniques for percutaneous coronary intervention.
TRA is the technique of choice for management of acute coronary syndrome (ACS) as it has significantly lower incidence of bleeding and vascular complications compared with the TFA approach.
TRA also has a mortality benefit for high risk ACS patients and high risk bleeding patients.
TRA was also found to yield improved quality of life, as well as decreased healthcare costs and resources.
Risks and complications
Embolization, or the launching of debris into the bloodstream.
Bleeding from over-inflation of a balloon catheter or the use of an inappropriately large or stiff balloon, or the presence of a calcified target vessel.
Hematoma or pseudoaneurysm formation at the access site.
Radiation-induced injuries (burns) from the X-rays used.
Contrast-induced renal injury.
Angioplasty may also provide a less durable treatment for atherosclerosis and be more prone to restenosis relative to vascular bypass or coronary artery bypass grafting.
Drug-eluting balloon angioplasty has significantly less restenosis, late lumen loss and target lesion revascularization at both short term and midterm follow-up compared to uncoated balloon angioplasty for femoropopliteal arterial occlusive disease.
Patients with stents are usually prescribed dual antiplatelet therapy (DAPT) which consists of a P2Y12 inhibitor, such as clopidogrel, which is taken at the same time as acetylsalicylic acid (aspirin).
Dual antiplatelet therapy (DAPT) is recommended for 1 month following bare metal stent placement, for 3 months following a second generation drug-eluting stent placement, and for 6–12 months following a first generation drug-eluting stent placement.
DAPT’s antiplatelet properties are intended to prevent blood clots, however they increase the risk of bleeding.
The concomitant use of Clopidogrel and Proton Pump Inhibitors following coronary angiography is associated with significantly higher adverse cardiovascular complications such as major adverse cardiovascular events (MACE), stent thrombosis and myocardial infarction.
Bare metal stents cause in-stent restenosis as a result of neointimal hyperplasia and stent thrombosis, which led to the invention of drug-eluting stents with anti-proliferative drugs to combat in-stent restenosis.
There is an inverse relationship between hospital primary angioplasty volume and mortality in patients with ST segment elevation MI (STEMI) (Canto JG).
National Registry Myocardial Infarction data analysis between 1994 in 1998 revealed that a higher primary angioplasty volume hospitals with greater than 33 procedures per year had a 28% lower in hospital mortality compared with low volume hospitals (Canto JG).
Contemporary studies in patients with STEMI analyzing 29,513 patient’s who underwent primary angioplasty indicated that compared with low and medium volume centers high volume centers had a better median door to balloon times, more use of evidence based therapies, but no improvement in length of stay or mortality(Get With The guidelines Steering Committee and Investigators).
The use of balloon angioplasty was limited by abrupt vessel closure due to dissections and restenosis.
Angioplasty carried out shortly after an MI has a risk of causing a stroke.
The mortality rate during angioplasty is 1.2%.
Sometimes chest pain can occur during angioplasty because the balloon briefly blocks off the blood supply to the heart.
The risk of complications with angioplasty is higher in:
People aged 65 and older
People who have kidney disease or diabetes
Women
People who have poor pumping function in their hearts
People who have extensive heart disease and blockages
Restenosis occurs in 30-40% of patients within 6 months after balloon angioplasty and in 20-30% of patients after angioplasty followed by stenting.
Percutaneous coronary balloon revascularization has a lower success rate and higher stenosis rate in small coronary artery than in larger vessels.
Warfarin before coronary angioplasty with a target INR of 2.1 to 4.8 leads to the lowest event rate, without an increase in bleeding episodes.
Comparison of angioplasty and medical therapy for coronary artery disease reveal that angioplasty improves exercise performance and reduces coronary symptoms to a greater extent than standard medical therapy, but may be associated with a slightly increased rate of major cardiac events such as myocardial infarction and death.
Has advantages compared to thrombolysis which include higher recanalization rates, immediate verification of procedural result, provides information about left ventricular function, and superior survival and reinfarction rates.
The American College of Cardiology/American Heart Association recommends primary angioplasty in patients with STEMI be conducted by laboratories performing at least 36 primary angioplasties a year, as well as 200 total angioplasty to a year (Antman EM).
Peripheral angioplasty refers to the use of a balloon to open a blood vessel outside the coronary arteries.
It is most commonly done to treat atherosclerotic narrowings of the abdomen, leg and renal arteries caused by peripheral artery disease.
Peripheral angioplasty is used in conjunction with guide wire, peripheral stenting and an atherectomy.
Angioplasty can be used to treat advanced peripheral artery disease to relieve the claudication, or leg pain, that is classically associated with chronic limb threatening ischemia.
