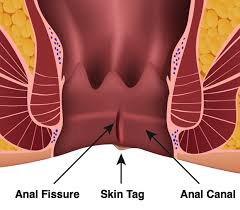
 Refers to a tear in the anoderm extending from the dentate line to the anal verge.
Refers to a tear in the anoderm extending from the dentate line to the anal verge.
Approximately 342,000 new cases of anal fissure disease are reported each year.
Most commonly affects younger and middle-age patients.
AF can be acute or chronic, that is present for greater than eight weeks.
Caused by the passage of hard stool or prolonged diarrhea which tear the anoderm.
Its pathophysiology is thought to be related to anal trauma, such as passage of hard stools, irritation from diarrhea, and anal rectal procedures.
A fissure begins as a small tear in the skin of the anal canal
The tear is then an exposed to internal sphincter muscle spasms which increases anal sphincter tone that compromises blood flow and leads to pressure induced ischemia that affects the midline portion of the anus, which receives less bloodflow than other areas.
The cycle of increased sphincter tone, and poor blood flow leads to decreased likelihood of healing and contributes to the development of chronic anal fissures from fibrosed edges..
Most are located in the posterior midline with the remainder located in the anterior midline.
It is a tear in the anoderm distal to the dentate line.
It causes severe, sharp pain associated with defecation that can result in debilitation.
Anal fissures are a common anorectal problems and typically occurs secondary to local trauma to the anoderm caused by the passage of hard stool.
Only 1% of fissures in men are located anteriorly while almost 20% of women’s lesions are so located.
Lesions in the lateral position suggest that other etiologies must be considered.
It may be associated with bright red rectal bleeding during and shortly after bowel movements because of local trauma to the anus.
The amount of localized anal rectal bleeding and mucoid discharge is variable in hemorrhoidal disease, whereas in anal fissures, bleeding is scant and mucoid discharge is usually absent.
Distinguishing between hemorrhoidal disease and anal fissures is difficult because patients present with many of the same overlapping symptoms, it is important because the management of the two conditions are very different.
Severe pain on rectal insertion of an examination finger may be a clue to diagnosis of anal fissure.
The presence of severe pain and tenderness preclude a complete anal rectal examination, making diagnosis difficult.
About 90% of cases are located in the posterior midline, but 25% of female and 8% of male patients, the fissures may be in located in the anterior midline.
Chronic fishers may be associated with the skin tag at the distal aspect of the Fisher, referred to as a sentinel tag.
Patients frequently have increased anal sphincter tone and tenderness with palpation near the fissure.
Some patients will not be able to tolerate a bedside rectal exam due to the severe pain.
Rarely a rectal examination under anesthesia may be required.
Small branches of inferior rectal arteries have minmal flow in the posterior commissure in 85% of patients indicating that the blood flow to the anoderm reflects the location of the tear and difficulty for the lesion to heal.
Pain causes internal sphincter spasm which increases pressure and further decreases blood flow and creates ischemia that inhibits healing of the lesion.
Patients present with severe pain upon defecation.
Patients frequently report tearing pain associated with passage of stool withnvisible blood on toilet paper and in the toilet after defecation.
Nonoperative management is the mainstay of treatment.
Non-operative therapy include: warm sits baths, psyllium fiber, other bulking agents, topical nitrates, calcium channel blockers, and botulinum toxin.
With with chronic anal fissures 0.2% nitroglycerin ointment most widely used drug treatment with 60-70% of cases healing within eight weeks.
Differential diagnoses:
Atypical fissure, such as those located laterally, and multiple fissures be caused by Crohn’s disease, HIV, tuberculosis, syphilis, or malignancy.
Perineal abscess
Anal fissure syndromes how frequently misattributed to hemorrhoids by patients and physicians up to 35% of the time.
Management includes avoiding further trauma to the anus and promoting relaxation of the internal anal sphincter by introducing dietary fiber and increasing water intake to enhance the bulk of stools.
Sitting in a warm-water bath 2-3 times a day is also recommended.
Opioids should be avoided due to constipation and exacerbation of symptoms.
Topical lidocaine is not effective managing anal fissures.
Topical agents of calcium channel blockers or topical nitrates cause smooth muscle relaxation and vasodilation and promote fissure healing by enhancing blood flow.
The persistence to recurrence of anal fissures despite conservative management suggests surgical treatments are indicated.
Botulinum toxin binds to presynaptic nerve terminals of the neuromuscular junction, resulting in sphincter relaxation and when injected into the anal sphincter has rates of healing similar to topical agents.
Surgery typically involves lateral internal sphincterotomy where the internal sphincter muscle is divided to relieve hypertonicity.
The lateral internal sphincterotomy is effective with durable results in long-term healing rates of more than 90%.
The lateral internal sphincterotomy is associated with possible recurrence an anal incontinence.
Following a lateral internal sphincterotomy, the recurrence rate of anal fissures is 6% and incontinence ranges from 3.4-4.4%.
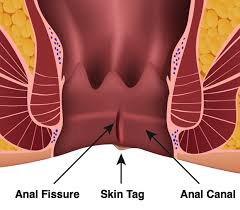 Refers to a tear in the anoderm extending from the dentate line to the anal verge.
Refers to a tear in the anoderm extending from the dentate line to the anal verge.