 Secretin hormone regulates water homeostasis throughout the body and influences the environment of the duodenum by regulating secretions in the stomach, pancreas, and liver.
Secretin hormone regulates water homeostasis throughout the body and influences the environment of the duodenum by regulating secretions in the stomach, pancreas, and liver.
It is a peptide hormone produced in the S cells of the duodenum, which are located in the intestinal glands.
Secretin is synthesized in cytoplasmic secretory granules of S-cells, which are found mainly in the mucosa of the duodenum, and in smaller numbers in the jejunum of the small intestine.
The secretin peptide is encoded by the SCT gene.
Gene location-Chromosome 11 (human)
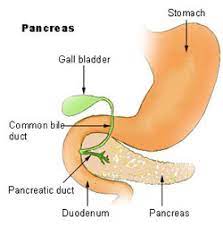
Secretin helps regulate the pH of the duodenum by (1) inhibiting the secretion of gastric acid from the parietal cells of the stomach and (2) stimulating the production of bicarbonate from the ductal cells of the pancreas.
Secretin stimulates the secretion of bicarbonate and water by cholangiocytes in the bile duct, protecting it from bile acids by controlling the pH and promoting the flow in the duct.
With secretin’s actions, the other main hormone simultaneously issued by the duodenum, cholecystokinin (CCK), stimulates the gallbladder to contract, delivering its stored bile.
Prosecretin is a precursor to secretin, which is present in digestion. Secretin is stored in this unusable form, and is activated by gastric acid.
This indirectly results in the neutralisation of duodenal pH, thus ensuring no damage is done to the small intestine by the aforementioned acid.
Secretin is initially synthesized as a 120 amino acid precursor protein known as prosecretin.
Secretin plays a role in osmoregulation by acting on the hypothalamus, pituitary gland, and kidney.
The secretin hormone is composed of 27 amino acids and has a molecular weight of 3055.
The amino acids sequences of secretin are similar to that of glucagon, vasoactive intestinal peptide (VIP), and gastric inhibitory peptide (GIP).
Secretin is released into circulation/ intestinal lumen in response to low duodenal pH that ranges between 2 and 4.5.
The acidity is due to hydrochloric acid in the chyme that enters the duodenum from the stomach via the pyloric sphincter.
The secretion of secretin is also increased by the products of protein digestion bathing the mucosa of the upper small intestine.
Secretin release is inhibited by H2 antagonists, which reduce gastric acid secretion.
As a result, if the pH in the duodenum increases above 4.5, secretin cannot be released.
Secretin primary functions to neutralize the pH in the duodenum, allowing digestive enzymes pancreatic amylase and pancreatic lipase
to function optimally.
Secretin targets the pancreatic centroacinar cells that have secretin receptors in their plasma membrane.
As secretin binds to these receptors, stimulating adenylate cyclase activity and converts ATP to cyclic AMP.
Cyclic AMP acts a an intracellular signal transduction and causes the organ to secrete a bicarbonate-rich fluid that flows into the intestine.
Bicarbonate is a base that neutralizes the acid, thus establishing a pH favorable to the action of other digestive enzymes in the small intestine.
Secretin also increases water and bicarbonate secretion from duodenal Brunner’s glands to buffer the incoming protons of the acidic chyme,and also reduces acid secretion by parietal cells of the stomach.
Secretin stimulates release of somatostatin, inhibits release of gastrin in the pyloric antrum, and downregulates the parietal cell acid secretory mechanics.
Secretin counteracts blood glucose concentration spikes by triggering increased insulin release from pancreas, following oral glucose intake.
Secretin modulates water and electrolyte transport in pancreatic duct cells, liver cholangiocytes, epididymis epithelial cells, and plays a role in the vasopressin-independent regulation of renal water reabsorption.
Secretin is found in the neurons of the paraventricular and supraoptic nuclei of the hypothalamus and along the neurohypophysial tract to neurohypophysis.
Secretin is released from the posterior pituitary during increased osmolality, and activates vasopressin release in the hypothalamus.
Secretin is needed to carry out the central effects of angiotensin II.
In nephrogenic diabetes insipidus abnormal secretin release could explain the abnormalities underlying this type syndrome of inappropriate antidiuretic hormone hypersecretion (SIADH).
In these individuals, vasopressin release and response are normal, although abnormal renal expression, translocation of aquaporin 2, or both are found.
Secretin is used in a diagnostic tests for pancreatic function.
Secretin is injected and the pancreatic output can then be imaged with magnetic resonance imaging, a noninvasive procedure, or secretions generated as a result can gathered either through an endoscope or through tubes inserted through the mouth, down into the duodenum.
A recombinant human secretin has been available for diagnostic purposes.
