 Thirteen vitamins necessary for health.
Thirteen vitamins necessary for health.
Vitamins A, C, D, E, K, thiamine (B1), riboflavin (B2), niacin (B3), pantothenic acid (B5), vitamin B6 (e.g., pyridoxine), biotin (B7), folate (B9), and cobalamin (B12).
Multivitamin use to improve longevity has not been supported by studies.
In an observation study of 390,100 adults use of multivitamins resulted in a small increase in risk mortality in a long term followup.
Vitamins and minerals are known as micronutrients.
Vitamins are organic molecules essential for an organism that are not classified as amino acids or fatty acids.
Approximately 30% of Americans use supplemental vitamins in the believe they will prevent and treat chronic diseases.
Although vitamin D deficiency is uncommon there are more than $20 million in annual sales for multivitamins?
Some vitamins can be produced from precursors they consume: vitamin A is synthesized from beta carotene; and niacin is synthesized from the amino acid tryptophan.
The term does not include the three other groups of essential nutrients: minerals, essential fatty acids, and essential amino acids.
Most vitamins are groups of related molecules called vitamers.
They commonly function as enzymatic cofactors, metabolic regulators or antioxidants.
Vitamins are classified as either water-soluble or fat-soluble.
There are 13 vitamins: 4 fat-soluble, A, D, E, and K, and 9 water-soluble, 8 B vitamins and vitamin C.
Water-soluble vitamins dissolve easily in water and, in general, are readily excreted from the body.
Because water soluble vitamins are not as readily stored, more consistent intake is important.
Fat-soluble vitamins are absorbed through the intestinal tract with the help of lipids.
Vitamins A and D can accumulate in the body, which can result in dangerous hypervitaminosis.
Urinary output is a strong predictor of vitamin consumption.
Vitamin E consists of four tocopherols and four tocotrienols.
There are thirteen vitamins required by human metabolism.
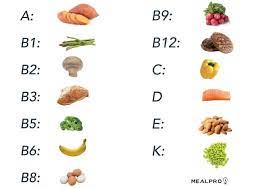
vitamin A
vitamin B1 (thiamine)
vitamin B2 (riboflavin)
vitamin B3 (niacin)
vitamin B5 (pantothenic acid)
vitamin B6 (pyridoxine)
vitamin B7 (biotin)
vitamin B9 (folic acid or folate)
vitamin B12 (cobalamins)
vitamin C (ascorbic acid)
vitamin D (calciferols)
vitamin E (tocopherols and tocotrienols)
vitamin K (quinones).
Vitamins have diverse biochemical functions.
Vitamin A acts as a regulator of cell and tissue growth and differentiation.
Vitamin D provides a hormone-like function, regulating mineral metabolism for bones and other organs.
The B complex vitamins function as coenzymes or the precursors for them.
Vitamins C and E function as antioxidants.
A deficiency or excess of a vitamin can potentially cause clinical illness.
Excess intake of water-soluble vitamins is less likely to cause illness.
Governments mandated the addition of vitamins to staple foods such as flour or milk, ref2242ed to as food fortification, to prevent deficiencies.
Folic acid supplementation during pregnancy reduces risk of infant neural tube defects.
Vitamin supplementation is of little value for healthy people who are consuming a vitamin-adequate diet.
Deficiency of vitamin A associated with night blindness, hyperkeratosis, and keratomalacia.
Sources of vitamin A-Fish in general, liver and dairy products; from plant origin as provitamin A / all-trans-beta-carotene: orange, ripe yellow fruits, leafy vegetables, carrots, pumpkin, squash, spinach.
Vitamin B1 Thiamine
Deficiency associated with Beriberi, Wernicke-Korsakoff syndrome Drowsiness and muscle relaxation
Sources-Pork, oatmeal, brown rice, vegetables, potatoes, liver, eggs
Vitamin B2 Riboflavin
Deficiency associated with Ariboflavinosis, glossitis, and angular stomatitis.
Riboflavin intake: Dairy products, bananas, green beans, asparagus.
Vitamin B3 Niacin
Deficiency associated with pellagra.
Liver damage occurs with doses > 2g/day.
Meat, fish, eggs, many vegetables, mushrooms, tree nuts are sources.
Vitamin B5 Pantothenic acid
Deficiency associated with Paresthesia and diarrhea, nausea and heartburn.
Foods with Vitamin B5 Meat, broccoli, avocados.
Vitamin B6 Pyridoxine.
Deficiency associated with anemia, Peripheral neuropathy, Impairment of proprioception, and nerve damage.
Foods containing pyridoxine- Meat, vegetables, tree nuts, bananas
Vitamin B7 Biotin
Deficiency associated with dermatitis, enteritis.
Biotin in raw egg yolk, liver, peanuts, leafy green vegetables.
Vitamin B9 Folate, Folic acid
Deficiency associated with megaloblastic anemia and deficiency during pregnancy is associated with birth defects, such as neural tube defects, and it may mask symptoms of vitamin B12 deficiency.
Found in leafy vegetables, pasta, bread, cereal, liver.
Vitamin B12 Cyanocobalamin
Deficiency associated with Pernicious anemia.
Found in Meat, poultry, fish, eggs, milk.
Vitamin C Ascorbic acid
Associated with Scurvy
Contained in many fruits and vegetables, liver.
Vitamin D Cholecalciferol (D3).
Deficiency associated with rickets and osteomalacia.
Found in Lichen, eggs, liver, certain fish species such as sardines, certain mushroom species such as shiitake
Vitamin E Tocopherols
Deficiency is very rare.
Associated with mild hemolytic anemia in newborn infants, and possible increased incidence of congestive heart failure.
Found in many fruits and vegetables, nuts and seeds, and seed oils.
Vitamin K
Deficiency associated with bleeding diathesis,decreased anticoagulation effect of warfarin.
Found in leafy green vegetables such as spinach, egg yolks, liver.
Fat-soluble vitamin deficiency due to malabsorption may be seen in cystic fibrosis.
They are essential for the normal growth and development.
A fetus develops from the nutrients it absorbs, and requires certain vitamins and minerals to be present at certain times.
Vitamins remain essential nutrients for the healthy maintenance of the cells, tissues, organs, and help increase the efficient use of chemical energy provided by food intake, and helps process proteins, carbohydrates, and fats required for cellular respiration.
Vitamin storage varies widely; vitamins A, D, and B12 are stored in significant amounts, mainly in the liver.
A diet deficient in vitamins A and D for many months and B12 in some cases for years, before developing a deficiency condition.
Vitamin B3 (niacin and niacinamide) is not stored in significant amounts, so stores may last only a couple of weeks
For vitamin C, the first symptoms of scurvy vary widely, from a month to more than six months, depending on previous dietary history that determined body stores.
Deficiencies of vitamins are classified as either primary or secondary.
A primary deficiency occurs when there is not enough of the vitamin in its food.
A secondary vitamin deficiency may be due to an underlying disorder that prevents or limits the absorption or use of the vitamin.
Smoking, excessive alcohol consumption, or the use of medications may interfere with the absorption or use of the vitamin.
People who eat a varied diet are unlikely to develop a severe primary vitamin deficiency.
In a national food and supplement survey conducted in the US over 2003-2006: over 90% of individuals who did not consume vitamin supplements were found to have inadequate levels of some of the essential vitamins, notably vitamins D and E.
Some vitamins have documented acute or chronic toxicity at larger intakes, ref2242ed to as hypertoxicity.
Consuming too much of any vitamin from food is remote.
Excessive intake of vitamins from dietary supplements does occur.
In 2016, overdose exposure to all formulations of vitamins and multi-vitamin/mineral formulations was reported by 63,931 individuals to the American Association of Poison Control Centers.
72% of the above exposures occurred in children under the age of five.
About 7% of adult supplement users exceeded the daily requirement for folate and 5% of those older than age 50 years exceeded the limit for vitamin A.
Water-soluble vitamins such as B and C dissolve into water when a vegetable is boiled: they are lost when the water is discarded.
RDA US Recommended Dietary Allowances; higher for adults than for children, and may be even higher for women who are pregnant or lactating.
There is little evidence that supplements have any benefits with respect to cancer or heart disease.
Vitamin A and E supplements not only provide no health benefits.
Vitamin A and E supplements may increase mortality, though the two large studies that support this conclusion included smokers for whom it was already known that beta-carotene supplements can be harmful.
A 2018 meta-analysis found no evidence that intake of vitamin D or calcium for community-dwelling elderly people reduced bone fractures.
Dietary supplements often contain vitamins, but may also include other ingredients, such as minerals, herbs, and botanicals.
A, D, E, K are fat soluble and the remainder are water soluble.
Fat soluble vitamins are more readily stored in the body than water soluble vitamins.
Fat soluble vitamins more likely to be poorly absorbed in gastrointestinal malabsorption disorders.
Small amount of some vitamins can be made endogenously-vitamin D from precursor steroids, vitamin K and biotin by intestinal microflora, and niacin from tryptophan, with the remainder of vitamins supplied from the diet.
Water-soluble vitamins include vitamin B-2 (riboflavin), B-3 (niacin), B-5 (pantothenic acid), B-6 (pyridoxine), B-7 (biotin, vitamin H), B-9 (folic acid), B-12 (cobalamin), and C (L-ascorbic acid).
Water soluble vitamins are stored in the body in limited quantities and therefore require regular replenishment through dietary intake.
Hypervitaminosis of water-soluble vitamins is rare.
Deficiencies may be dietary, that is, primary or secondary in nature related to intestinal malabsorption, impaired blood transport, storage or metabolic conversion.
Deficiency of a single vitamin is unusual.
Digestion and absorption of carotenes and retinoids require bile, pancreatic enzymes and some levels of antioxidant activity in food.
Use of dietary supplements is not associated with mortality benefits.
The Western Norway B Vitamin Intervention Trial (WENBIT), a prospective, randomized, double blind, placebo controlled secondary prevention study of the clinical effects of B vitamins-B12, folic acid and vitamin B6, in patients having undergone coronary angiography for suspected CAD or aortic valve stenosis: results indicated no effect of treatment on total mortality, or cardiovascular events ands their use cannot support their use for secondary prevention inpatients with coronary artery disease.
In an analysis of 18 studies including 2,019,862 participants with 18,363,326 person-years of follow-up, there was no association between vitamin supplementation and CVD, coronary heart disease (CHD), or stroke mortality, even after adjusting for duration of supplement use, lifestyle risk factors, and demographics (Kim, J).
The researchers also found that supplementation was associated with a lower risk for CHD incidence, though this finding was not significant in the pooled analysis of randomized controlled trials.
Women’s health initiative found that multivitamin use did not reduce the risk of cancer, including colorectal cancer (Newhouser ML et al).
Multivitamins are the most common dietary supplement.
Multivitamins are taken regularly by at least one third of US adults.
Multivitamin use is growing and as many as 53% of Americans report daily use.
Multivitamin supplementation has failed to improve cognition in older men, to reduce cardiovascular events in patients with previous myocardial infarction and has no effect on cancer risk on mortality.
The traditional role of daily multivitamin therapy is to prevent nutritional deficiency.
The combination of multivitamins and minerals, contained in multivitamin preparations, may mirror healthy dietary patterns such as fruit and vegetable intake, which is been modestly and inversely associated with cancer risk in some studies.
In general trials of high dose individual vitamins and minerals for cancer has had lack of effect.
For a health population there is no evidence in support of the recommendation for the use of multivitamin/mineral supplements the primary prevention of chronic disease.
The self reported use of 15 vitamins and minerals supplements in relation to 38,772 women in the Iowa Women’s Health Study was associated with higher risk of total mortality, and supplemental iron was strongly and dose dependently associated with increased risk of mortality while supplemental calcium was associated with a decreased risk.
Multivitamin use during and after adjuvant chemotherapy for colorectal cancer in patients with stage IIIa disease was not associated with improved outcomes (Ng K et al).
In a randomized double blind controlled trial of high-dose versus standard dose multivitamin supplementation for 24 months and 3418 patients with HIV initiating HAART therapy: there was no decrease in HIV disease progression or death, but they may have been an increase in ALT levels (Isanaka S et al).
The Physicians Health Study II is a randomized, double-blind trial testing the long-term effects of common multivitamins in the prevention of chronic disease.
In the above study 14,641 male US physicians enrolled in a common vitamin study beginning in 1997 with treatment and follow-up through 2011: it was an associated reduction in total cancers among men with baseline history of cancer, but did not differ significantly among men initially without cancer.
In a study in northern China of an undernourished population of 3318 individuals age 40-69 years with a previous cytologic diagnosis of esophageal squamous dysphasia and who were followed for 20 additional years: There was no effect on total or cause specific mortality, demmonstrating little benefit of multivitamin supplementation on mortality in either well or poorly nourished populations (Wang J-B et al).
