
 Most common manifestation of osteoporosis.
Most common manifestation of osteoporosis.
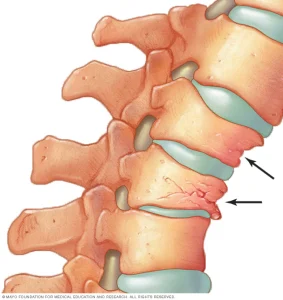
Vertebral fractures are the most common osteoporotic fractures and account for 70% of all fractures.
One in 5 women with an asymptomatic or symptomatic vertebral fracture will experience another vertebral fracture within one year.
Presence of a vertebral fracture also increases risk of nonvertebral fractures.
Vertebral fractures of the thoracic and lumbar spine account for almost half of the 1.5 million osteoporotic fractures that occur annually.
Can result in acute and chronic pain, decreases the quality of life and diminishes lifespan.
Are robust predictators of future fractures
The majority of vertebral fractures do not come to clinical attention.
Usually diagnosed clinically with complaints of back pain, and x-rays confirming fracture of a thoracolumbar transition zone or midthoracic region.
Most vertebral fractures are not noted clinically at the time of their occurrence.
Accounts for more than 150,000 hospitalizations per year.
Only 25-33% of radiographically diagnosed VF are clinically diagnosed.
Estimated 25% postmenopausal women have a vertebral fracture, and the prevalence increases with age.
Incidence increasing substantially in men and women especially if the 75 years, we were is the incidence of hip fracture is declining.
Associated with advanced age, lower bone mineral density, falling, smoking, inadequate calcium intake.
A vertebral fracture is a strong predictor of subsequent fractures, both vertebral and nonvertebral.
Whether symptomatic or radiographically identified, are associated with increased mortality and morbidity, including back pain and decreased activity, with consequent increased days of bed rest.
Severity and number of VFs associated with likelihood of back pain and impaired quality of life.
Newly diagnosed VF by radiographic changes associiated with back pain and back-pain related disability.
Lumbar fractures associated with greater disabilities than thoracic fractures.
Increased risk of death associated with VFs due to associated conditions that are associated with vertebral fractures and death.
Clinical and radiographic VFs associated with increased risk of osteoporotic fractures, such as hip fravtures and this risk is only in part explained by lowered bone mineral density.
Risk of vertebral fracture is increased among women in whom a prior fracture is identified.
Approximately 20% of women will experience another fracture within the first year of a vertebral fracture.
Most common osteoporotic fracture in postmenopausal women, and two thirds of them are not recognized to have occurred.
In patients with multiple vertebral fractures restrictive lung disease, chronic pain, early satiety and impaired self esteem may occur.
Asymptomatic vertebral fractures associated with decreased quality of life, increased likelihood for hospitalization and increased mortality rates.
Prevalence and incidence of radiographic VFs increase with age.
Prevalence in white women increases from 5% to 10% between ages 50 and 59.
Prevalence 30% or more in white women at 80 years of age or older.
Rates lower in Black women, Asian women and men compared to white women.
Among women 65 years or older without a VF, there is an annual risk of fracture of 0.9%, among those 80 years or older the annual risk is 1.7% (Nevitt MC et al).
Clinical guidelines recommend pharmacologic therapy, regardless of bone mineral density in old individual with a new vertebral fracture.
