
The umbilical cord, also called the navel string, birth cord or funiculus umbilicalis.
Refers to a conduit between the developing embryo or fetus and the placenta.
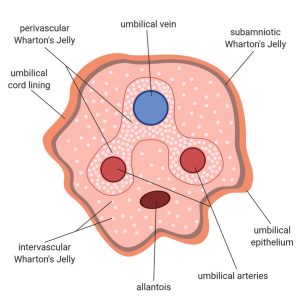
During prenatal development, the umbilical cord is physiologically and genetically part of the fetus and contains two arteries and one vein.
The two arteries, the umbilical arteries, and one vein, the umbilical vein, are buried within Wharton’s jelly.
The umbilical vein supplies the fetus with oxygenated, nutrient-rich blood from the placenta.
The fetal heart pumps deoxygenated, nutrient-depleted blood through the umbilical arteries back to the placenta.
Vaginal ultrasonography of an embryo of a gestational age of 8 weeks and 3 days identifies the embryo is surrounded by the thin membranes of the amniotic sac, with the umbilical cord is seen in the center, attaching the embryo to the placenta.
The umbilical cord develops from and contains remnants of the yolk sac and allantois.
The umbilical cord forms by the fifth week of fetal development, replacing the yolk sac as the source of nutrients for the fetus.
The cord is not directly connected to the mother’s circulatory system.
The cord but joins the placenta, which transfers materials to and from the mother’s blood without allowing direct mixing.
The length of the umbilical cord is approximately equal to the crown-rump length of the fetus throughout pregnancy.
The umbilical cord in a full term neonate is usually about 20 inches long and about 0.75 in diameter.
The umbilical cord diameter decreases rapidly within the placenta.
The fully patent umbilical artery has two main layers: an outer layer consisting of circularly arranged smooth muscle cells and an inner layer which shows rather irregularly and loosely arranged cells embedded in abundant ground substance.
The umbilical cord contains Wharton’s jelly, a gelatinous substance made largely from mucopolysaccharides which protects the blood vessels inside.
Delayed umbilical cord clamping in term neonates resulted in improved neonatal hemoglobin levels at 24-48 hours of life, improved iron stores at 3-6 months of age, and improved neurodevelopmental indices through age 4.
The UC contains one vein, which carries oxygenated, nutrient-rich blood to the fetus, and two arteries that carry deoxygenated, nutrient-depleted blood away.
Occasionally, only two vessels, one vein and one artery, are present in the umbilical cord.
It is unusual for a vein to carry oxygenated blood and for arteries to carry deoxygenated blood, and also occurs with the pulmonary veins and arteries, connecting the lungs to the heart.
The umbilical vein carries blood towards the fetus’s heart, while the umbilical arteries carry blood away.
The blood flow through the umbilical cord is approximately 35 ml / min at 20 weeks, and 240 ml / min at 40 weeks of gestation.
The blood flow through the umbilical cord is approximately 115 ml / min / kg of weight at 20 weeks and 64 ml / min / kg at 40 weeks.
The umbilical cord enters the fetus via the abdomen, at the point which will become the umbilicus or navel after separation.
Within the fetus, the umbilical vein continues towards the liver, where it splits into two.
One of the umbilical vein branches joins with the hepatic portal vein, which carries blood into the liver.
The second branch, the ductus venosus, bypasses the liver and flows into the inferior vena cava, which carries blood towards the heart.
The two umbilical arteries branch out from the internal iliac arteries.
The umbilical arteries pass on either side of the urinary bladder into the umbilical cord, completing the circuit back to the placenta.
The umbilical cord occludes physiologically shortly after birth, explained both by a swelling and collapse of Wharton’s jelly in response to a reduction in temperature and by vasoconstriction of the blood vessels by smooth muscle contraction.
A natural clamp occurs halting the flow of blood.
In air this physiological clamping will take three minutes or less.
In water birth, where the water temperature is close to body temperature, normal pulsation can be 5 minutes and longer.
Closure of the umbilical artery by vasoconstriction occurs as multiple constrictions which increase both in number and degree with time.
The vasoconstrictive occlusion appears to be mainly mediated by 5-hydroxytryptamine and thromboxane A2.
In umbilical cords of preterm infants the artery contracts more to angiotensin II and arachidonic acid and is more sensitive to oxytocin than in term ones.
The umbilical vein and ductus venosus in the newborn close up, and degenerate into fibrous remnants known as the round ligament of the liver and the ligamentum venosum respectively.
Part of each umbilical artery closes up, degenerating into what are known as the medial umbilical ligaments.
Remaining umbilical artery sections are retained as part of the circulatory system.
A number of abnormalities can affect the umbilical cord, which can cause problems that affect both mother and child:
Umbilical cord compression from entanglement of the cord,a knot in the cord, or a nuchal cord,
Velamentous cord insertion
Single umbilical artery
Umbilical cord prolapse
Vasa praevia
Compressions do not always cause obstruction of fetal circulation.
Delaying the clamping of the umbilical cord until one minute after birth improves outcomes.
Clamping of the cord is followed by cutting of the cord.
Cutting of the cord is painless due to the absence of nerves.
The cord is extremely tough, and cutting it requires a sharp instrument.
There is ordinarily no significant loss of either venous or arterial blood while cutting the cord.
Uumbilical cord clamp are safer and faster than knives.
After the cord is clamped and cut, the newborn wears a plastic clip on the navel area until the compressed region of the cord has dried and sealed sufficiently.
The length of cord left attached after clamping and cutting is minimal, and the remaining umbilical stub remains for up to 10 days as it dries and then falls off.
A Cochrane review in 2013 concluded that delayed cord clamping between one and three minutes after birth as contrasted to early, resulted in no difference in risk of severe maternal postpartum hemorrhage or neonatal mortality.
Delayed clamping results in an increased birth weight of on average about 100 g, and an increased hemoglobin concentration of on average 1.5 g/dL with half the risk of being iron deficient at three and six months, but an increased risk of jaundice requiring phototherapy.
In 2012, the American College of Obstetricians and Gynecologistsk endorsed delaying clamping of the umbilical cord for 30–60 seconds with the newborn held below the level of the placenta in all cases of preterm delivery based largely on evidence that it reduces the risk of intraventricular hemorrhage by 50%.
There is an increased risk of polycythemia and hyperbilirubinemia associated with delayed clamping..
A meta-analysis showed that delaying clamping of the umbilical cord in full-term neonates for a minimum of 2 minutes following birth is beneficial to the newborn in giving improved hematocrit, iron status, stored iron, as well as a reduction in the risk of anemia.
Negative effects of delayed cord clamping include an increased risk of polycythemia, which appears benign.
A higher rate of neonatal jaundice requires phototherapy.
Delayed clamping is not recommended where the newborn is not breathing well and needs resuscitation.
In such a situation the recommendation is to immediately clamp and cut the cord and perform cardiopulmonary resuscitation.
Omitting cord severance entirely, a practice called “lotus birth” or umbilical nonseverance, allows the cord to dry and separate on its own, typically on the 3rd day after birth.
As the umbilical vein which is directly connected to the central circulation can be used as a route for placement of a venous catheter for infusion and medication.
The umbilical vein catheterization is an alternative to percutaneous peripheral or central venous catheters or intraosseous canulas and may be employed in resuscitation or intensive care of the newborn.
The blood within the umbilical cord, known as cord blood.
Cord blood is an available source of primitive, undifferentiated stem cells of type which are CD34-positive and CD38-negative.
These cord blood cells can be used for bone marrow transplant.
Diverting blood from the baby’s umbilical blood through early cord clamping and cutting, to freeze for long-term storage at a cord blood bank should the child ever require the cord blood stem cells.
Critics assert that early cord blood withdrawal at the time of birth actually increases the likelihood of childhood disease, due to the high volume of blood taken with an average of 108ml in relation to the baby’s total supply, typically 300ml.
In multiple studies, cancer-causing chemicals have been found in the blood of umbilical cords.
Chemicals in the blood of umbilical cords originate from plastics, computer circuit boards, fumes and synthetic fragrances, with more than 300 toxic chemicals have been found.
Blacks, Hispanics, and Asians, and the poor tend to have higher rates of chemicals obsoleted from umbilical cord blood.
Contamination can lead to omphalitis associated with purulent material, redness and swelling that can lead to sepsis and death in the newborn.
Antiseptic applications reduce bacterial colonization and infections.
Omphalitis incidence in developing countries ranges from 2-77 per 100,000 hospital born infants.
Chlorhexidine is the favored topical antimicrobial with activity against gram-positive and gram-negative organisms, proven safety and effectiveness.
Use of chlorhexidine markedly reduces the incidence of omphalitis.
