 Incidence increasing over the last four decades: by 313%.
Incidence increasing over the last four decades: by 313%.
Recently the incident rate is stabilized, likely due to more conservative indications for thyroid biopsy and re-classification of noninvasive follicular thyroid neoplasms with papillary like features.
For the US population lifetime risk of being diagnosed with thyroid carcinoma is 1.2%.
Approximately 44,000 new cases are diagnosed each year with the five-year relative survival of 98.5%.
Most thyroid cancer risk factors, are non-modifiable: age, sex, race, ethnicity, and family history.
Advancing age is associated with increased incidence and poor survival.
Hereditary forms of well-differentiated thyroid cancer occur in 3-9% of thyroid cancer cases.
It was estimated that 43,720 new cases of thyroid carcinoma would be diagnosed in the US in 2023, with 2,230 deaths.
Thyroid carcinomas occur more often in women, however mortality rates are lower for younger women.
Thyroid cancer is the ninth most common cancer worldwide, the seventh most common cancer in US women and the most common cancer in adolescents and adults younger than 40 years.
The incidence rate is more than three fold higher in women.
Increased incidence is a result of increased use of diagnostic imaging and surveillance.
Increased incidence due to increased diagnosis of papillary cancer.
The exposure to ionizing radiation in childhood has the strongest association who is papillary thyroid cancer.
Mortality rates for thyroid cancer have remained low at 0.5 per hundred thousand US persons per year and the five-year relative survival rate of 98.5%.
Anaplastic thyroid cancer represents only 1% of all thyroid cancers, but contributes 19.9% of the annual thyroid cancer, related mortality, and a median survival of 6.5 months.
Papillary thyroid carcinoma cancer, accounts for approximately 84% of all thyroid cancers.
Follicular thyroid cancer accounts for about 4%, and oncocytic thyroid cancer accounts for around 2%.
Papillary, follicular and oncocytic thyroid cancers are termed well-differentiated thyroid cancer.
Non-toxic nodular goiter is associated with an increased risk of thyroid cancer.
Higher preoperative serum thyroid levels is associated with thyroid cancer, in patients undergoing thyroid surgery for unilateral or bilateral thyroid nodules, large thyroid glands, or autoimmune thyroid disease.
Less common and more aggressive sub types of thyroid cancer include poorly differentiated, and anaplastic thyroid carcinoma that arise from well differentiated thyroid cancer, after accumulation of genetic mutations.
Medullary thyroid carcinoma accounts for 4% of thyroid cancers and arises from parafollicular C cells.
Accounts for 90% of endocrine cancers.
Lifelong risk is less than 1% with 0.83% for women and 0.33% for men (Horner MJ et al).
Incidence rate in the United States has risen from 4.9 cases per 100,000 persons in 1975 to 14.3 cases per 100,000 persons in 2014.
Fifth most common cancer in women in the US.
Estimated 62,980 new cases in 2014 and 1,890 deaths in 2014.
The five year relative survival, a weighted average of all stages of the disease is 98.5%, with approximately 2100 thyroid cancer deaths estimated per year in the United States.
Thyroid cancer is has an indolent course with an excellent prognosis in most cases resulting in a recommendation against screening, mitigating overdetection.
Ranks 10th in incidence among solid organ malignancies.
16th most common cancer worldwide with about 298,000 new cases diagnosed globally in 2012.
Death due to thyroid cancer is relatively rare, with a mortality rate of approximately 0.5 deaths per hundred thousand individuals.
The stable age and gender adjusted mortality rate for thyroid carcinoma contrasts with the declining rates for other solid tumors and adults.
Incidence among men has risen more dramatically than any other malignancy in recent years with a 2.4% annual increase.
SEER data- among 77,276 patients in the registry with thyroid cancer, the mean age was 48 years, 75% were women, and 82% were Caucasian.
In the above study 84% were papillary thyroid cancers and 11% follicular thyroid cancers.
Except for medullary, thyroid carcinoma, which arises from neural crest, derived parafollicular, C cells, thyroid carcinomas are derived from thyroid follicular epithelial cells.
Highest incidence is reported in North America.
Estimated 62,450 cases of differentiated thyroid cancer was diagnosed in USA in 2015.
Incidence 2008 13.22 per 100,000 persons.
Over 400,000 people living with TC in the US.
While the incidence is increasing, the mortality rate has changed minimally over the past five decades.
Challenge is to treat thyroid cancers by balancing the therapeutic approach so that patients with lower risk disease or Benign thyroid nodules are not overtreated.
It is essential to recognize patients who have more advanced to high risk disease and who need aggressive treatment.
Clinical behavior is very from indolent tumors with low mortality in most cases, to very aggressive malignancies such as anplastic thyroid cancer.
DNA sequencing studies reveal the genetic basis of most thyroid cancers.
Most thyroid cancers harbor mutations along the mitogen-activated protein kinase (MAPK) cellular signaling pathway, transmitting growth signals from the plasma membrane to the nucleus and plays a central role in the regulation of cellular proliferation.
The main histological types: differentiated-papillary, follicular, and Hurthle cell: Medullary: and anaplastic.
Papillary carcinomas make up 88%, follicular 5.5%, Hurthle cell 2.3%, medullary thyroid cancer 1.8%, and anaplastic carcinoma make up 0.9% of thyroid cancers
Death rate increasing at a rate second to deaths from cancer of the liver and intrahepatic bile ducts.
Dfferentiated thyroid carcinomas usually have an excellent prognosis, with a 10 year survival rate exceeding 90 to 95%.
Anaplastic thyroid carcinoma is almost uniformly lethal.
Since differentiated thyroid carcinomas represent more than 95% of all cases, most thyroid carcinoma deaths are from papillary, follicular, and Hurthle cell carcinomas.
Strong female predominance 3.0:1.
Rare in children below the age of 10 years.
Increase in incidence mostly due to new cases of papillary thyroid cancer, with relative decrease in other types.
Most patients die from other than thyroid cancer.
10 years survival for localized thyroid cancer confined to the thyroid is close to 100%.
Papillary carcinoma accounts for 90% of pediatric thyroid cancers.
Children with thyroid cancer usually present with more extensive thyroid disease than adults, and more than 80% have lymph node metastases, and 10-20% have lung metastases.
Children have excellent prognosis despite more advanced disease, with most having long-term survival.
Childhood thyroid cancer may be more responsive to thyroid suppression, or have a greater avidity to iodine and tend to have RET/PTC rearrangements.
Adults with papillary thyroid cancer often have BRAF mutation which may be associated with tumor recurrence and decreased iodine avidity.
Oncogenic molecular alterations have been documented in up to 90% of thyroid carcinomas.
BRAF is the most commonly mutated gene reported in 60% of papillary, 35% of high-grade thyroid carcinomas, and 45% of anaplastic thyroid carcinomas.
RAS mutations are dominant in follicular thyroid cancer at 30 to 45%, present in 10 to 20% of papillary thyroid carcinomas, 20% to 40% of high-grade thyroid carcinomas, and 10 to 20% of anaplastic thyroid carcinomas.
Gene fusion events are oncogene abnormalities in a subset of thyroid carcinomas.
Most cases arise from thyroid follicular cells.
Arise from follicular or para-follicular cells.
Differentiated and undifferentiated tumor is originated in follicular cells.
Vast majority are papillary (88%) or follicular (9%)-differentiated cancers.
Majority of lesions are differentiated cancers which includes papillary, follicular, and Hurthle cell variants.
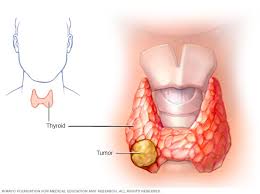
Diagnosis: thyroid nodules may be detected on physical exam or found incidentally, undiagnosed imaging studies.
The prevalence of palpable thyroid nodules is across 5% in women, and 1% in men who live in iodine sufficient areas of the world.
Ultrasound can detect thyroid nodules in 19 to 68% of randomly selected patients: thyroid nodules are more common in women at 40.6% men in men about 28%.
Approximately 7–15% of thyroid nodules are malignant.
Determination of malignancy is based on ultrasound characteristics and cytological analysis.
Evaluation of patients with thyroid nodules, larger than 1 cm, by cytology or ultrasound confirm malignancy in one percent of patients.
Recommendations are not to biopsy nodules smaller than 1 cm.
Ultrasound characteristics include: nodule size, echogenicity, borders, vascularity, and the presence of calcifications: sensitivity for detecting malignancy is 64 to 77% and specificity is 82 to 90% with ultrasound.
Most patients with differentiated thyroid carcinoma can be cured, with a 5 year survival rate of 97.8%.
Anaplastic thyroid cancer is the most uniformly fatal type of far right cancer, but most carcinoma depths are from papillary, follicular, and Hurthle cell carcinomas, which account for 95% of all thyroid cancers.
Poorly differentiated or undifferentiated thyroid cancers include anaplastic thyroid cancer.
Thyroid cancer occurs more often in women, but mortality rates are higher in men, because of an older age at diagnosis.
Medullary thyroid cancer is arise from parafollicular or C cells and may be familial or sporadic.
Medullary thyroid cancer comprises 2-3% of all thyroid cancers.
Following surgery thyroid hormone is administered to compensate for the function of the resected thyroid disease and to prevent recurrence.
Strong association with pregnancy, especially with spontaneous or induced abortions.
Serum thyroglobulin measurements are the most sensitive indicators of recurrent disease.
Previous radiation exposure to the head and neck area is related to less favorable pathologic and clinical outcome in patients after surgical management (Seaberg R).
30-50% of adults patients with well differentiated thyroid cancer have palpable nodal disease.
Up to 90% of patients with well-differentiated disease have histologically proven lymph node metastases after elective modified radical neck dissection.
Before treatment with radioiodine it is standard practice to reduce the body’s stores of iodine by avoiding iodine rich diet and supplements which may contain iodine.
Most patients with differentiated forms of thyroid cancer are managed successfully with surgery, radioactive iodine and long-term thyroid hormone suppression treatment.
Most well differentiated fibroid cancers are at low risk of recurrence and can be cured with surgery alone.
Preoperative, neck ultrasound, evaluates the thyroid central and lateral neck compartments, while CT of the neck with contrast or MRI is reserved for patients with large tumors, suspected extrathyroid extension, lymph node metastases or aggressive histology.
Patients undergoing surgery should have preoperative assessment of the vocal cords.
For unilateral, well differentiated thyroid, cancer, small than 4 cm thyroid, lobectomy is preferred as survival is equivalent to that with total thyroidectomy,
Complications of hypoparathyroidism are less frequent with thyroid lobectomy.
Overall survival of patients undergoing thyroid lobectomy is equivalent to patients undergoing total thyroidectomy.
Total thyroidectomyrecommended for well differentiate thyroid cancer 4 cm or larger or for bilateral thyroid cancer disease.
Following thyroidectomy for well differentiated thyroid cancer to ensure full eradication of remnant thyroid tissue and to treat microscopic residual disease, and patients with visible, inoperable, iodine avid metastases radioactive iodine is often administered.
Lobectomy versus total thyroidectomy:most studies show the extent of surgery is not associated with overall survival for unifocal, node negative, non-metastatic tumors up to 4 cm in size.
Survival after partial thyroidectomy is similar to survival if the total thyroidectomy for patients at low and high risk.
Most specialists advocate for unilateral lobectomy as an appropriate management for most patients with papillary and follicular carcinoma based on low mortality and low recurrence rates among these patients and the high complication rate dissociate with more extensive thyroidectomy.
10 year survival rate among patients with metastatic thyroid cancer that retains radioiodine avidity is approximately 60%, and it is only 10% if metastases arenrefractory to radioiodine therapy.
For well differentiated advanced iodine avid thyroid cancer the administration of radioactive iodine results in reduced tumor recurrence and improved survival.
For patients with a well differentiated very low risk thyroid cancer treatment with radioactive iodine is of uncertain benefit.
Differentiated carcinomas of the thyroid had a 20 year overall survival of almost 90%.
25 to 50% of patients with locally advanced or metastatic disease will become refractory to radioactive iodine.
Poorly differentiated thyroid cancer is having less radioactive avidity and anaplastic undifferentiated lesions or refractory to radioactive iodine.
When the patient develops RAI refractory differentiated thyroid cancer, the chances of survival markedly decreases compared with patients who are radio active iodine sensitive.
The 10 year survival rate was 92% among patients who responded to radioactive iodine but dropped to 19% in patients who did not (Durante C et al).
RAI refractory patients may have disease in the neck, distant metastases, or both and may ultimately died from the process.
Associated with several genetic alterations including the RET proto-oncogene, which coats were 80 cell membrane receptor tyrosine kinase.
RET proto-oncogene expressed in parafollicular C cells but not in follicular cells.
RET proto-oncogene can be activated in follicular cells by chromosomal translocation RET/PTC rearrangement.
RET/PTC is found at approximately 20% of adults sporadic papillary carcinoma patients.
An RET point mutation is commonly found in parafollicular C cells derived medullary thyroid cancers.
25-50% of metastatic differentiated thyroid cancers can lose functional iodine concentrating ability to become in sensitive to radioactive iodine therapy: When this occurs less than 50% of patients will be alive at 3 years (Wang W).
B-RAF kinase (BRAF) can activate the mitogen activated protein kinase (MAPK) signaling pathway, and point mutation was of the BRAF gene are found and 45% of thyroid papillary cancers.
PET scans can localize sites of metastases and demonstrate radioactive iodine resistance, as thyroid carcinomas were low iodine and daily at higher glucose metabolism and are more likely to be positive on PET scans.
Radioactive iodine has little or no therapeutic effect on PET scan positive tumors and tumors that concentrate radioactive iodine are not likely to be active on PET scan.
FDG avidity is the most practical and reproducible definition of radioactive iodine resistance disease in thyroid cancer with a median sensitivity and specificity of 77% in 78%, respectively.
Indeterminate cytology occurs in 30% of cases and molecular testing can define the diagnosis.
RAS point mutations also activate the MAPK signaling pathway and occurs in all types of thyroid follicular cell adenomas and carcinomas, suggesting RAS hasn’t role in the early tumor genesis of thyroid cancer.
Mutations of 1 of 3 genes: RET/PTC,BRAF,or RAS are found in greater than 70% of papillary carcinomas and they rarely overlap in the same malignancy.
The most common genetic variants are associated with and promote growth of thyroid cancer occur in proteins of the intracellular mitogen – activated, protein kinase (MAPK) pathway.
The most common gene variant is BRAF V600E found in approximately 60% of patients with papillary thyroid cancer.
Doxorubicin shows little effectiveness and significant toxicity in refactory thyroid cancer.
Presently multi kinase inhibitors are available for progressive differentiated thyroid cancer refractory to radioactive iodine and include sorafenib and lenvatinib.
In a double-blind, placebo controlled phase 2 trial of 417 patients treated with radioactive iodine refractory thyroid cancer, locally advanced or metastatic differentiated thyroid cancer given sorafenib 400 mg b.i.d. or placebo:median progression free survival was 10.8 months and 5.8 months for placebo.
Multi kinase inhibitors for progressive differentiated thyroid cancer refractory to radioactive iodine eventually fail.
The United States Preventive Services Task Force (USPSTF) has recommended against screening asymptomatic individuals for thyroid cancer (grade D recommendation).
The incidence rate of thyroid cancer in the United States has risen from 4.9 cases per 100,000 persons in 1975 to 14.3 cases per 100,000 persons in 2014.
Despite this, however, the mortality rate has remained stable at about 0.5 deaths per 100,000 persons.
There is inadequate direct evidence to determine whether screening in asymptomatic individuals improved outcomes, but that the magnitude of benefit is no greater than small.
USPSTF has recommended against screening for thyroid cancer in asymptomatic adults, but does not apply to individuals at increased risk of thyroid cancer due to a history of high radiation exposure, inherited genetic syndromes, or hisotry of thyroid cancer.
Thyroid ultrasound criteria for malignancy include: solid aspect, hypoechogenicity, taller then wide shape, irregular margin, extrathyroidal extension, calcification, and punctate echogenic foci.
Patient with suspected thyroid cancer undergo fine needle aspiration biopsy or surgical resection which is assessed by pathological examination.
Thyroid nodules smaller than 1 cm and thyroid nodules smaller than 1.5 cm, with without, ultrasound features suspicious for malignancy should be monitored with ultrasound rather than biopsied.
Observation without surgery may be appropriate in selective patients with small papillary, thyroid cancers.
History of patients with biopsy proven well differentiated thyroid cancer, less than 1 cm followed without surgical resection for a medium of six years and up to 15 years, only 15.9% of microcarcinomas grew by 3 mm or more, and 3.4% of patients develop cervical node metastasis at 10 years and none developed distant metastasis at 10 years..
Sorafenib, lenvatinib, vandetanib TKI’s have been the mainstay of treatment for iodine refractory well differentiated thyroid cancer.
Most persistent or recurrent well differentiated, thyroid cancer detected in the neck in the first five years after initial thyroidectomy with a median time to recurrence of 3.6 years.
Surgical management is the preferred treatment for local regional disease and external beam radiation is also considered in unresectible cancer or suspected microscopic persistent disease, but is rarely indicated.
Only 5% of patients have distant metastatic disease either at presentation or during the course of the disease.
Mortality differs by organ siteeffect the five year survival is 77% in patients with lung metastases, and in patients with bone and liver metastasis the five year survival is 25% and 21%, respectively.
Most patients refractory to radioiodine therapy with well differentiated thyroid cancer, and those with recurrent or metastatic cancer have indolent disease and do not need immediate treatment with systemic therapy.
Multiple agents or combinations of agents are approved for thyroid cancer: sorafenib. lenvatinob, vandetinib, cabozanitinib, entrectinib, larotrectinob, dabtafenib/trametinib: multikinase inhibitors, and targeted agents.
