A rare malignant disease with incidence about 0.02 per hundred thousand person-years.
Fewer than 100 cases are diagnosed annually in the US.
Patients are typically 50 to 70 years of age at presentation.
Categorized as type C thymomas.
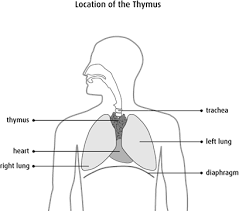
The majority of these lesions are a squamous cell carcinoma that penetrate the thin thymic epithelial capsule, invade mediastinal structures, and disseminate to the pleura.
These tumors which arise from the epithelium of the thymus are associated with paraneoplastic syndrome in 30 to 40% of thymoma cases and up to 5% of thymic carcinoma cases, with myasthenia gravis the most common complication.
PET scan: standardized uptake value (SUV) for thymic carcinoma is considered to be significantly greater than that for invasive or noninvasive thymoma, often with an SUV cutoff point of 5.0, thymic carcinoma can be differentiated from thymoma with reasonably high sensitivity (84.6%), specificity (92.3%), and accuracy (88.5%).
Differential diagnosis: aggressive mediastinal germ cell tumor,
primary mediastinal lymphoma with invasive spread: lack infiltration
lung cancer with mediastinal invasion
Maximal surgical resection is typically recommended for localized thymic carcinoma.
Radiotherapy is supported by large retrospective studies associated with improved outcomes.
With macroscopic growth outside the capsule of the thymus or invasion of surrounding mediastinal structures platinum based chemotherapy can debulk prior to surgery if indicated, with adjuvant radiation to reduce the risk of recurrence.
Cytotoxic chemotherapy program, death ligand checkpoint immunotherapy are other measures.
Durable responses with the above treatments have been observed in 15 to 20% of patients.
