A T cell is a type of lymphocyte.
T cells play a central role in the adaptive immune response.
T cells are distinguished from other lymphocytes by the presence of a T-cell receptor (TCR) on their cell surface.
T cells originate from hematopoietic stem cells, found in the bone marrow.
These T cells migrate to the thymus gland to mature.
The precursor cells mature into several distinct types of T cells.
T cell differentiation continues after leaving the thymus, and specific differentiated T cell subtypes have roles controlling and shaping the immune response.
T cell functions include immune-mediated cell death.
immune-mediated cell death is carried out by two major subtypes: CD8+ killer and CD4+ helper T cells.
These T cells are named for the presence of the cell surface proteins CD8 or CD4.
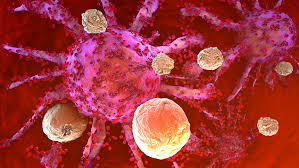
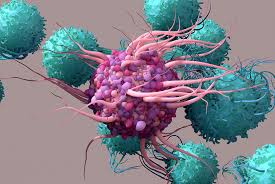
CD8+ T cells, killer T cells.are cytotoxic, and are able to directly kill virus-infected cells, as well as cancer cells.
CD8+ T cells are also able to use small signaling proteins, known as cytokines, to recruit other types of cells when mounting an immune response.
The CD4+ T cells, function as helper cells.
Unlike CD8+ killer T cells, these CD4+ helper T cells function by indirectly killing cells identified as foreign: they determine if and how other parts of the immune system respond to a specific, perceived threat.
Helper T cells use cytokine signaling to influence regulatory B cells directly, and other cell populations indirectly.
Regulatory T cells provide the critical mechanism of tolerance, whereby immune cells are able to distinguish invading cells from self.
Regulatory T cells prevent immune cells from inappropriately reacting against ones’ own cells, known as an “autoimmune” response.
Regulatory T cells have also been called “suppressor” T cells.
Regulatory T cells can also be co-opted by cancer cells to prevent the recognition of, and an immune response against, tumor cells.
All T cells originate from hematopoietic stem cells (HSC) which reside in the bone marrow.
Hematopoietic stem cells subsequently differentiate into multi potent progenitors which retain the ability to become both myeloid and lymphoid cells.
The lymphoid progenitor can only differentiate into T, B or NK cells.
These cells then migrate via the blood to the thymus, where they engraft.
The earliest lymphoid progenitor cells arriving at the thymus are called double-negative, as they do not express either the CD4 or CD8 co-receptor.
The early committed cells are CD4-CD8-CD44+CD25-ckit+ thymic progenitor cells.
Mature T cells will contain a unique TCR that reacts to a random pattern, allowing the immune system to recognize many different types of pathogens.
The TCR consists of two major components, the alpha and beta chains.
T cells must show that their TCR can recognize the body’s MHC complex and that it does not react to self proteins.
Double-positive thymocytes (CD4+/CD8+) migrate deep into the thymic cortex, where they are presented with self-antigens expressed by thymic cortical epithelial cells on MHC molecules.
Thymocytes that interact with MHC-I or MHC-II receive a vital survival signal.
The selected T cells have an MHC affinity enabling them to interact with MHC and peptide complexes to effect immune responses.
The vast majority of developing thymocytes die during this process.
Double-positive cells are CD4+/CD8+, that interact well with MHC class II molecules and will eventually become CD4+ cells, whereas thymocytes that interact well with MHC class I molecules mature into CD8+ cells.
A T cell becomes a CD4+ cell by down-regulating expression of its CD8 cell surface receptors.
Potentially autoimmune cells are removed by negative selection, which occurs in the thymic medulla.
Negative selection removes thymocytes that are capable of strongly binding with self MHC peptides.
Thymocytes that survive positive selection migrate towards the boundary of the cortex and medulla in the thymus.
Thymocytes that interact too strongly with the self-antigen receive an apoptotic signal that leads to cell death.
Some of these cells are selected to become Treg cells.
The remaining cells exit the thymus as mature naïve T cells and those process is a component of central tolerance and serves to prevent the formation of self-reactive T cells that are capable of inducing autoimmune diseases in the host.
In the medulla negative selection obliterates T cells that bind too strongly to self-antigens expressed on MHC molecules, allowing for tolerance of self by the immune system.
T cells that leave the thymus are self-restricted, self-tolerant, and single positive.
About 98% of thymocytes die during the development processes in the thymus by failing positive or negative selection.
2% of thymocytes survive and leave the thymus to become mature immunocompetent T cells.
The thymus contributes fewer T cells as a person ages.
The thymus shrinks by about 3% a year throughout middle age, with a corresponding fall in the thymic production of naïve T cells.
This leaving peripheral T cell expansion and regeneration to play a greater role in protecting older people.
T cells are grouped into a series of subsets based on their function. CD4 and CD8 T cells are selected in the thymus, but undergo further differentiation in the periphery to specialized cells which have different functions.
T cell subsets were initially defined by function, but also have associated gene or protein expression patterns.
T helper cells (TH cells) assist other lymphocytes, including maturation of B cells into plasma cells and memory B cells, and activation of cytotoxic T cells and macrophages.
T helper cells (TH cells) are also known as CD4+ T cells as they express the CD4 on their surfaces.
Helper T cells become activated when they are presented with peptide antigens by MHC class II molecules, which are expressed on the surface of antigen-presenting cells (APCs).
Once activated Helper T cells divide rapidly and secrete cytokines that regulate or assist the immune response.
Cytokines direct T cells into particular subtypes.
CD4+ Helper T cell subsets
Cytotoxic T cells (TC cells, CTLs, T-killer cells, killer T cells) destroy virus-infected cells and tumor cells, and are also implicated in transplant rejection.
Cytotoxic T cells are defined by the expression of the CD8 protein on their cell surface.
Cytotoxic T cells bind to short 8-11 peptide amino acids associated with MHC class I molecules, present on the surface of all nucleated cells.
Cytotoxic T cells also produce the key cytokines IL-2 and IFNγ, which
influence the effector functions of other cells, in particular macrophages and NK cells.
Antigen-naïve T cells expand and differentiate into memory and effector T cells after they encounter an antigen within the context of an MHC molecule on the surface of a professional antigen presenting cell, a dendritic cell.
Populations of memory T cells were discovered including tissue-resident memory T (Trm) cells, stem memory TSCM cells, and virtual memory T cells.
All memory T cell subtypes are long-lived and can quickly expand to large numbers of effector T cells upon re-exposure to their antigen, providing the immune system with “memory” against previously encountered pathogens.
Memory T cells may be either CD4+ or CD8+ and usually express CD45RO.
Central memory T cells (TCM cells) express CD45RO, C-C chemokine receptor type 7 (CCR7), and L-selectin (CD62L).
Central memory T cells also have intermediate to high expression of CD44.
Effector memory T cells (TEM cells and TEMRA cells) express CD45RO but lack expression of CCR7 and L-selectin.
Effector memory T cells (TEM cells and TEMRA cells) have intermediate to high expression of CD44.
These memory T cells lack lymph node-homing receptors and are thus found in the peripheral circulation and tissues.
Regulatory T cells are required for the maintenance of immunological tolerance.
Regulatory T cells shut down T cell-mediated immunity toward the end of an immune reaction and to suppress autoreactive T cells that escaped the process of negative selection in the thymus.
Two major classes of CD4+ Treg cells have been described — FOXP3+ Treg cells and FOXP3− Treg cells.
Regulatory T cells can develop either during normal development in the thymus, and are then known as thymic Treg cells, or can be induced peripherally and are called peripherally derived Treg cells.
Both subsets require the expression of the transcription factor FOXP3.
Mutations of the FOXP3 gene can prevent regulatory T cell development, causing the fatal autoimmune disease IPEX.
Other types of T cell have suppressive activity, but do not express FOXP3.
These include Tr1 cells and Th3 cells, which originate during an immune response and act by producing suppressive molecules.
Tr1 cells are associated with IL-10, and Th3 cells are associated with TGF-beta.
Natural killer T cells bridge the adaptive immune system with the innate immune system.
Conventional T cells that recognize protein peptide antigens presented by major histocompatibility complex (MHC) molecules, while NKT cells recognize glycolipid antigens presented by CD1d.
Activated T cells can perform functions ascribed to both helper and cytotoxic T cells: cytokine production and release of cytolytic/cell killing molecules, and are also able to recognize and eliminate some tumor cells and cells infected with herpes viruses.
Mucosal associated invariant T cell (MAIT) cells display innate, effector-like qualities.
Gamma delta T cells (γδ T cells) represent a subset of T cells which possess a γδ TCR rather than the αβ TCR on the cell surface.
The majority of T cells express αβ TCR chains.
Gamma delta T cells (γδ T cells) are found mostly in the gut mucosa, within a population of intraepithelial lymphocytes.
T cells contribute to immune defenses in two major ways.
Some T cells direct and regulate immune responses; others directly attack infected or cancerous cells.
Activation of CD4+ T cells occurs through the simultaneous engagement of the T-cell receptor and a co-stimulatory molecule (like CD28, or ICOS) on the T cell by the major histocompatibility complex (MHCII) peptide and co-stimulatory molecules on the APC.
Both are required for production of an effective immune response; in the absence of co-stimulation, T cell receptor signalling alone results in anergy.
Optimal CD8+ T cell response relies on CD4+ signalling.
CD4+ cells are useful in the initial antigenic activation of naïve CD8 T cells, and sustaining memory CD8+ T cells in the aftermath of an acute infection.
Therefore, activation of CD4+ T cells can be beneficial to the action of CD8+ T cells.
The first signal is provided by binding of the T cell receptor to its cognate peptide presented on MHCII on an APC.
The second signal comes from co-stimulation, in which surface receptors on the APC are induced by a relatively small number of stimuli, usually products of pathogens, but sometimes breakdown products of cells, such as necrotic-bodies or heat shock proteins.
The only co-stimulatory receptor expressed constitutively by naïve T cells is CD28, so co-stimulation for these cells comes from the CD80 and CD86 proteins, which together constitute the B7 protein, (B7.1 and B7.2, respectively) on the APC.
Receptors expressed upon activation of the T cell, such as OX40 and ICOS, largely depend upon CD28 for their expression.
The second signal allows the T cell to respond to an antigen, and without it, the T cell becomes anergic.
This mechanism prevents inappropriate responses to self.
When a T cell has been appropriately activated, it alters its cell surface expression of a variety of proteins.
Markers of T cell activation include CD69, CD71 and CD25 and HLA-DR.
CTLA-4 expression is also up-regulated on activated T cells, which in turn outcompetes CD28 for binding to the B7 proteins.
This is a checkpoint mechanism to prevent over activation of the T cell.
The T cell receptor exists as a complex of several proteins.
T cell activation is modulated by reactive oxygen species.
T cells have the ability to discriminate between healthy and abnormal (e.g. infected or cancerous) cells in the body.
Healthy cells typically express a large number of self derived pathological MHC on their cell surface and although the T cell antigen receptor can interact with at least a subset of these self pMHC, the T cell generally ignores these healthy cells.
However, when these very same cells contain even minute quantities of pathogen derived pMHC, T cells are able to become activated and initiate immune responses.
The ability of T cells to ignore healthy cells but respond when these same cells contain pathogen (or cancer) derived pMHC is known as antigen discrimination.
Causes of T cell deficiency include lymphocytopenia of T cells and/or defects on function of individual T cells.
Insufficiency of T cell function can result from hereditary conditions such as severe combined immunodeficiency.
Partial insufficiencies of T cell function include: acquired immune deficiency syndrome (AIDS), and hereditary conditions such as DiGeorge syndrome (DGS), chromosomal breakage syndromes (CBSs), and B cell and T cell combined disorders such as ataxia-telangiectasia (AT) and Wiskott–Aldrich syndrome (WAS).
Pathogens that are a concern in T cell deficiencies are intracellular pathogens, including Herpes simplex virus, Mycobacterium and Listeria.
Fungal infections are also more common and in T cell deficiencies.
T-cell lymphoma, and accounts for perhaps one in ten cases of non-Hodgkin lymphoma.
The main forms of T cell lymphoma are:
Extranodal T cell lymphoma
Cutaneous T cell lymphomas: Sézary syndrome and Mycosis fungoides
Anaplastic large cell lymphoma
Angioimmunoblastic T cell lymphoma
T cell exhaustion refers to the state of dysfunctional T cells, characterized by progressive loss of function, changes in transcriptional profiles and sustained expression of inhibitory receptors.
T cells at first cells lose their ability to produce IL-2 and TNFα followed by the loss of high proliferative capacity and cytotoxic potential, eventually leading to their deletion.
Exhausted T cells typically indicate higher levels of CD43, CD69 and inhibitory receptors combined with lower expression of CD62L and CD127.
Exhaustion can develop during chronic infections, sepsis and cancer.
Exhausted T cells preserve their functional exhaustion even after repeated antigen exposure.
T cell exhaustion can be triggered by several factors like persistent antigen exposure and lack of CD4 T cell help.
Antigen exposure also has effect on the course of exhaustion because longer exposure time and higher viral load increases the severity of T cell exhaustion.
At least 2–4 weeks exposure is needed to establish exhaustion.
Another factor able to induce exhaustion are inhibitory receptors including programmed cell death protein 1 (PD1), CTLA-4, T cell membrane protein-3 (TIM3), and lymphocyte activation gene 3 protein (LAG3).
Soluble molecules such as cytokines IL-10 or TGF-β are also able to trigger exhaustion.
Treg cells can be a source of IL-1can play a role in T cell exhaustion.
T cell exhaustion is reverted after depletion of Treg cells and blockade of PD1.
T cell exhaustion can also occur during sepsis as a result of cytokine storm.
Sepsis carries high antigen load and inflammation, increasing T cell exhaustion.
T cell exhaustion can develop following persistent antigen exposure after graft transplant.
T cell response diminishes over time after kidney transplant, suggesting T cell exhaustion plays an important role in tolerance of a graft mainly by depletion of alloreactive CD8 T cells.
Studies show positive effect of chronic infection on graft acceptance and its long-term survival mediated partly by T cell exhaustion.
Recipient T cell exhaustion provides sufficient conditions for NK cell transfer.
The induction of T cell exhaustion can be beneficial for transplantation it also carries disadvantages among which can be counted increased number of infections and the risk of tumor development.
During cancer T cell exhaustion plays a role in tumor protection.
According to research ome cancer-associated cells as well as tumor cells themselves can actively induce T cell exhaustion at the site of tumor.
T cell exhaustion can also play a role in cancer relapses n leukemia.
