 Produced by type II pneumocytes of the alveoli, and are contained in the osmiophilic lamellar bodies of such cells.
Produced by type II pneumocytes of the alveoli, and are contained in the osmiophilic lamellar bodies of such cells.
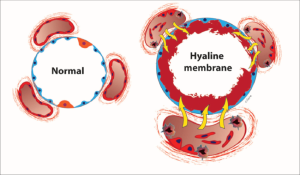
The lungs in respiratory distress syndrome are developmentally deficient in surfactant.
Surfactant helps prevent the collapse of the terminal air spaces, the future site of alveolar development, throughout the normal cycle of inhalation and exhalation.
The surfactant is packaged by the cell in structures called lamellar bodies, and extruded into the air spaces.
The lamellar bodies then unfold into a complex lining of the air space.
This layer reduces the surface tension of the fluid that lines the alveolar air space.
Surface tension is responsible for approximately 2/3 of the inward elastic recoil forces.
By reducing surface tension, surfactant prevents the air spaces from completely collapsing on exhalation.
The decreased surface tension allows reopening of the air space with a lower amount of force.
Without adequate amounts of surfactant, the air spaces collapse and are very difficult to expand.
Surfactant is normally in activated and/or depleted continuously and must be continuously secreted to maintain low surface tension and prevent atelectasis.
Surfactant’s stimulus to secrete is the mechanical stress resulting from stretching type II pneumocytes.
The sigh recruits more surfactant.
Surfactant deficiency is related to inhibition from the insulin that is produced in the newborn, especially those of diabetic mothers.
Pulmonary surfactant is a complex system of lipids, proteins and glycoproteins that is produced in specialized lung cells called Type II cells or Type II pneumocytes.
Surfactant reduces surface tension at the air-alveolar interface, thus preventing alveolar collapse, and plays a role in innate immunity.
A phospholipid, which serves to differentially reduce surface tension at different volumes, and contributes to alveolar stability.
Surfactant protein C is a hydrophobic peptide that functions in the presence of appropriate phospholipids, to lower surface tension at low lung volumes by facilitating the spreading and adsorption of the phospholipids extant at the air-liquid interface.
The protein itself is inserted into the phospholipid monolayer as a function of surface tension, facilitating respreading of surfactant after alveolar compression at low volumes and promotes surfactant recycling.
Choline is also needed for the synthesis of pulmonary surfactant, a mixture consisting mostly of phosphatidylcholines.
The surfactant is responsible for lung elasticity, that is for lung tissue’s ability to contract and expand: deficiency of phosphatidylcholines in the lung tissues has been linked to acute respiratory distress syndrome.
Produced beginning about the 24th week of gestation and is found in amniotic fluid between 28-32 weeks.
By week 35 most infants have sufficient amounts of surfactant.
Use decreases the mortality among very premature infants.
Use has not increased proportions of children with significant neurological disabilities.
Helps lower surface tension in the airways and helps keep alveoli open.
Preterm infants frequently treated with surfactant for respiratory distress syndrome, and it is usually administered via endotracheal tube during mechanical ventilation.
The application of surfactant to spontaneously breathing preterm infants receiving positive airway pressure, reduces the need for mechanical ventilation (Gopel W, et al).
