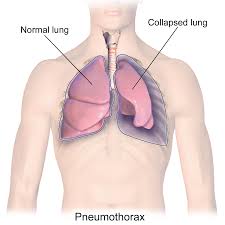
 Represents air trapped within the pleural space that develops without antecedent trauma.
Represents air trapped within the pleural space that develops without antecedent trauma.
Primary spontaneous pneumothorax patients have no previously identified underlying lung disease or chest trauma.
Overall incidence estimated at 17-24 per 100,000 in the male population and 1-6/100,000 in the female population.
1-6 year recurrence rates range from 17-54%.
Spontaneous pneumothorax recurrence rates approximately 26% within five years of initial primary spontaneous pneumothorax.
Approximately 75% of her recurrent pneumothoraces occur in the first year following the initial event.
Secondary spontaneous pneumothorax is the find as a spontaneous pneumothorax occurring in a patient with an established underlying lung disorder.
Male patients aged 15-34 with underlying chronic lung disorders have the highest probability of recurrent pneumothorax within five years at more than 39%.
The initial peak incidence occurs among patients age 15-34 years, the majority of whom have no previously identified lung disorders.
Younger age may be a significant risk factor for recurrent pneumothorax.
A subsequent peak in incidence occurs in men and women older than 60 years, many of whom have underlying lung disorders.
Smoking associated with a higher recurrence rate of spontaneous pneumothoraces
Interstitial lung disease and malignancy or significantly more common among patients aged 65 years or older compared with younger patients.
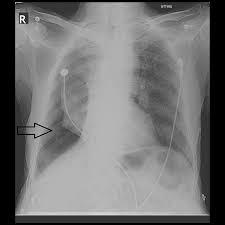
Management includes: observation, needle aspiration, chest tube drainage, endobronchial interventions, pleurodesis, and video assisted thoroscopic surgery.
Non-operative management is an option for minimally symptomatic patients.
For moderate to large primary spontaneous pneumothorax conservative management was non-inferior to interventional management, with a lower risk of serious adverse events (Brown SGA).
In the primary Spontaneous Pneumothorax Trial, conservative management of primary spontaneous pneumothorax has a favorable safety profile, and is not inferior to interventional management in the resolution of normal thorax.
Fndings in the above study found lung re-expansion at 8 weeks was 94.4% in a conservative management group and 98.5% in the intervention group.
Patients with secondary pneumothorax and pulmonary diseases warrant surgical treatment because of high recurrence rate (Savitsky E).
Patients with spontaneous pneumothorax should avoid air travel and other activities that could affect intrathoracic pressure for at least two weeks following complete resolution of the pneumothorax.
Patients with recurrent pneumothorax, contralateral pulmonary disease, or high risk occupations are typically treated with surgery.
Tube thoracostomy timing of chest tube removal depends on successful lung reexpansion without an air leak.
A persistent air leak requires more invasive therapeutic interventions.
