 Spondylosis is the degeneration of the vertebral column from any cause.
Spondylosis is the degeneration of the vertebral column from any cause.
It refers to spinal osteoarthritis, the age-related wear and tear of the spinal column, which is the most common cause of spondylosis.
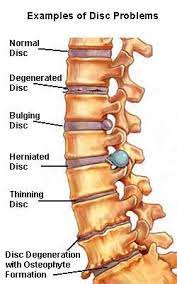
The spondylitis degenerative process chiefly affects the vertebral bodies, the neural foramina and the facet joints.
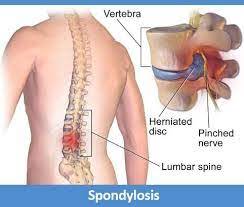
When severe spondylosis may cause pressure on the spinal cord or nerve roots with subsequent sensory or motor disturbances, such as pain, paresthesia, imbalance, and muscle weakness in the limbs.
The ompression of a nerve root emerging from the spinal cord may result in radiculopathy with sensory and motor disturbances, such as severe pain in the neck, shoulder, arm, back, or leg, accompanied by muscle weakness.
Direct pressure on the spinal cord, typically in the cervical spine, may result in myelopathy, characterized by global weakness, gait dysfunction, loss of balance, and loss of bowel or bladder control.
Shock-like paresthesias in hands and legs because of nerve compression and lack of blood flow.
Spondylitis of cervical vertebrae is labelled cervical spondylosis.
Lower back spondylosis is labeled lumbar spondylosis.
Rarely severe spondylosis can result in vertebrobasilar insufficiency, due to the vertebral artery becoming occluded as it passes up in the transverse foramen.
As the spinal joints stiffen in cervical spondylosis, the chondrocytes which maintain the disc become deprived of nutrition and die.
Secondary osteophytes may cause stenosis for spinal nerves, manifesting as radiculopathy.
Spondylosis is caused from years of constant abnormal pressure, caused by joint subluxation, stress induced by sports, acute and/or repetitive trauma, or poor posture, being placed on the vertebrae and the discs between them.
Such abnormal stresses causes the body to form new bone in order to compensate for the new weight distribution.
This abnormal weight bearing from bone displacement will cause spondylosis to occur.
Poor postures and loss of the normal spinal curves can lead to spondylosis as well.
Spondylosis can affect a person at any age; however, older people are more susceptible.
Techniques used in the diagnosis of spondylosis, these are;
Cervical Compression Test, a variant of Spurling’s test, is performed by laterally flexing the patient’s head and placing downward pressure on it.
Neck or shoulder pain on the ipsilateral side, the side to which the head is flexed, indicates a positive result for this test.
Lhermitte sign: feeling of electrical shock with patient neck flexion.
Reduced range of motion of the neck, the most frequent objective finding on physical examination.
While MRI and CT scans are helpful for pain diagnosis but generally are not definitive and must be considered together with physical examinations and history.
Treatment
Surgery is advocated for cervical radiculopathy in patients who have intractable pain, progressive symptoms, or weakness that fails to improve with conservative therapy.
Surgical indications for cervical spondylosis with myelopathy (CSM) remain somewhat controversial, but most clinicians recommend operative therapy over conservative therapy for moderate-to-severe myelopathy.
Physical therapy may be effective for restoring range of motion, flexibility and core strengthening,and decompressive therapies (i.e., manual mobilization, mechanical traction) may also help alleviate pain.
Current surgical procedures used to treat spondylosis aim to alleviate the signs and symptoms of the disease by decreasing pressure in the spinal canal and/or by controlling spine movement with fusion surgery, but the evidence is limited in support of some aspects of these procedures.
The vertebral column can be operated on from both an anterior and posterior approach.
Commonly, osteophytes and portions of intervertebral disc are removed.
Fusion surgery is performed when there is evidence of spinal instability or mal-alignment.
Use of instrumentation, such as pedicle screws, in fusion surgeries varies across studies.
