 2008
2008
1945
Starts caudally from the brain stem and gives off branches along the length of the spine.
The spinal cord is part of the central nervous system that supplies nerves and receives information from the peripheral nervous system within the body.
The spinal cord consists of grey and white matter and a central cavity, the central canal.
Blood supply is from 1 anterior and 2 posterior spinal arteries.
Its function is to carry information from the brain to different parts of the body.
Adjacent to each vertebra emerge spinal nerves.
The spinal nerves provide sympathetic nervous supply to the body, with nerves emerging forming the sympathetic trunk and the splanchnic nerves.
Segments include the cervical (C1-C8), Thoracic (T1-T12), Lumbar (L1-L5), Sacral (S1-S5), and Coccygeal.
In the cervical region the spinal cord levels share the same number as the spinal segment below it.
In other spinal segments the spine shares the same number as the spinal segment above it.
Each spinal cord segment receives sensory input from dermatomal regions of the body and sends motor output to myotomal regions.
Adjacent to each vertebra emerge spinal nerves.
The spinal nerves provide sympathetic nervous supply to the body, with nerves emerging forming the sympathetic trunk and the splanchnic nerves.
The cauda equina refers to the caudal end of the spinal cord where it splits into multiple motor and sensory roots which exit’s the vertebral canal through the lumbar intervertebral and sacral foramina.
The conus medullaris is the median cord remaining in the spine following the deviation of the cauda equina and terminates at L1 in adults and L3 in newborns.
The spinal column elongates much more than the spine cord so the spinal cord ends at a more cranial level in adults than in newborns.
A cauda equina syndrome is associated with preservation of sexual function, muscle atrophy, unilateral pain and areflexia with a slow progression process.
The conus medullaris is associated with sexual dysfunction, bilateral mild pain, Incontinence and preservation of reflexes.
A long, thin, tubular bundle of nervous tissue and support cells that extends from the medulla oblongata in the brainstem to the lumbar region of the vertebral column.
Together brain and spinal cord make up the central nervous system (CNS).
The spinal cord begins at the occipital bone and extends down to the space between the first and second lumbar vertebrae..
The spinal cord it does not extend the entire length of the vertebral column.
The spinal cord is around 45 cm (18 in) in men and around 43 cm (17 in) long in women.
The spinal cord varies in width, ranging from 13 mm (1⁄2 in) thick in the cervical and lumbar regions to 6.4 mm (1⁄4 in) thick in the thoracic area.
The bony vertebral column encloses no protects the relatively shorter spinal cord.
The spinal cord functions primarily in the transmission of neural signals between the brain and the rest of the body.
The spinal cord also contains neural circuits that can independently control numerous reflexes and central pattern generators.
Has three major functions: conduit for motor information, which travels down the spinal cord
as a conduit for sensory information in the reverse direction,
and as a center for coordinating certain reflexes.
It connects the brain to nerves throughout the body.
The main pathway for information connecting the brain and peripheral nervous system.
The length of the spinal cord is much shorter as compared to the length of the vertebral column, extending from the foramen magnum and continues through to the conus medullaris near the second lumbar vertebra, terminating in a fibrous extension known as the filum terminale.
The spinal cord is about 45 cm long in men in around 43 cm in women.
The spinal cord is ovoid shaped and is enlarged in the cervical and lumbar regions.
The cervical enlargement, is located from C5 to T1 spinal segments.
C1 through C4 split and recombine to produce nerves that serve the neck and back of head.
Spinal nerve C1 is called the suboccipital nerve, which provides motor innervation to muscles at the base of the skull.
C2 and C3 form many of the nerves of the neck, providing both sensory and motor control.
These include the greater occipital nerve, which provides sensation to the back of the head, the lesser occipital nerve, which provides sensation to the area behind the ears, the greater auricular nerve and the lesser auricular nerve.
The phrenic nerve is a nerve essential for our survival which arises from nerve roots C3, C4 and C5.
It supplies the thoracic diaphragm, enabling breathing.
If the spinal cord is transected above C3, then spontaneous breathing is not possible.
The cervical enlargement is the site where sensory input comes from and motor output goes to the arms.
The lumbar enlargement, is located between L1 and S3 spinal segments.
The lumbar enlargement manages sensory input and motor output coming from and going to the legs.
It is continuous with the caudal portion of the medulla, and it runs from the base of the skull to the body of the first lumbar vertebra.
The spinal cord does not run the full length of the vertebral column in adults.
It is made of 31 segments that each contain sensory nerve root and motor nerve root.
The first cervical segment is usually very small and may be absent.
Nerve roots merge into 31 bilaterally symmetric pairs of spinal nerves.
The peripheral nervous system is made up of these spinal roots, nerves, and ganglia.
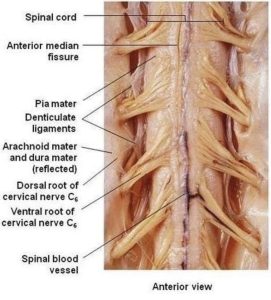
Dorsal roots are fascicles of axons in the spinal cord that receive sensory information from the skin, muscle, and visceral organs that enter through the dorsal root entry zone.
The dorsal root ganglia hold the cell bodies of dorsal root ganglia in the spinal ganglia related with that spinal segment.
Ventral roots only have efferent fibers that arise from motor neurons whose cell bodies are found in the ventral, or anterior, gray horns of the spinal cord.
The spinal cord is protected by three layers of membranes, the meninges, that surround the canal .
The dura mater is the outermost layer, and it forms a tough protective coating.
Between the dura mater and the surrounding bone of the vertebrae is the epidural space, which is filled with adipose tissue, and it contains a network of blood vessels.
The arachnoid mater is the middle protective layer. with its spiderweb-like appearance.
The space between the arachnoid and the underlying pia mater is called the subarachnoid space.
The subarachnoid space contains the cerebrospinal fluid (CSF).
A lumbar puncture withdrawing cerebrospinal fluid from the subarachnoid space, usually from the lumbar region of the spine.
The pia mater, the innermost protective layer is very delicate and it is tightly associated with the surface of the spinal cord.
The spinal cord is stabilized within the dura mater by the connecting denticulate ligaments, which extend from the pia mater laterally between the dorsal and ventral roots.
The dural sac ends at the vertebral level of the second sacral vertebra.
The periphery region of the cord contains neuronal white matter tracts containing sensory and motor neurons.
Internal to this peripheral region is the grey matter, containing the nerve cell bodies of the grey matter in the three grey columns of the spinal cord that give the region its butterfly-shape.
The central region surrounds the central canal, which is an extension of the fourth ventricle and contains cerebrospinal fluid.
The spinal cord has an elliptical shape.
The spinal cord has grooves in the dorsal and ventral sides, the posterior median sulcus is the groove in the dorsal side, and the anterior median fissure is the groove in the ventral side.
In the upper part of the vertebral column the spinal nerves exit directly from the spinal cord, whereas in the lower part of the vertebral column nerves pass further down the column before exiting.
The terminal portion of the spinal cord is called the conus medullaris, but the pia mater continues as an extension called the filum terminale, which anchors the spinal cord to the coccyx.
The cauda equina refers to the collection of nerves in the vertebral column that continue to travel through the vertebral column below the conus medullaris.
The cauda equina forms because the spinal cord stops growing in length at about age four, even though the vertebral column continues to lengthen until adulthood.
Sacral spinal nerves originate in the upper lumbar region.
The spinal cord can be anatomically divided into 31 spinal segments based on the origins of the spinal nerves.
Each segment of the spinal cord is associated with a pair of ganglia, called dorsal root ganglia.
The dorsal root ganglia are situated just outside the spinal cord, ganglia contain cell bodies of sensory neurons.
Ganglia cell body axon sensory neurons travel into the spinal cord via the dorsal roots.
Ventral roots consist of motor neuron axons, which bring information to the periphery from cell bodies within the CNS.
Dorsal roots and ventral roots join and exit the intervertebral foramina as they become spinal nerves.
The grey column, in the center of the cord, is shaped like a butterfly and consists of cell bodies of interneurons, motor neurons, neuroglia cells and unmyelinated axons.
The anterior and posterior grey column present as projections of the grey matter and are also known as the horns of the spinal cord.
The grey columns and the gray commissure form the grey H.
The white matter is located outside of the grey matter and consists almost totally of myelinated motor and sensory axons.
Columns of white matter carry information either up or down the spinal cord.
Within the CNS, nerve cell bodies are generally organized into clusters, called nuclei.
Axons within the CNS are grouped into tracts.
There are 31 spinal cord nerve segments in a human spinal cord:
8 cervical segments forming 8 pairs of cervical nerves.
The C1 spinal nerves exit spinal column between occiput and C1 vertebra.
C2 nerves exit between posterior arch of C1 vertebra and lamina of C2 vertebra.
C3–C8 spinal nerves through Foramina above corresponding cervica vertebra, with the exception of C8 pair which exit via foramina between C7 and T1 vertebra.
12 thoracic segments forming 12 pairs of thoracic nerves exit spinal column through Foramina below corresponding vertebra T1–T12.
5 lumbar segments forming 5 pairs of lumbar nerves exit spinal column through foramina, below corresponding vertebra L1–L5.
5 sacral segments forming 5 pairs of sacral nerves exit spinal column through foramina, below corresponding vertebra S1–S5.
There is 1 coccygeal segment
In the fetus, vertebral segments correspond with spinal cord segments.
Because the vertebral column grows longer than the spinal cord, spinal cord segments do not correspond to vertebral segments in the adult, particularly in the lower spinal cord.
Lumbar and sacral spinal cord segments are found between vertebral levels T9 and L2, and the spinal cord ends around the L1/L2 vertebral level.
The end of the spinal cord forms a structure known as the conus medullaris.
Although the spinal cord cell bodies end around the L1/L2 vertebral level, the spinal nerves for each segment exit at the level of the corresponding vertebra.
The lower spinal cord nerves exit the vertebral column much lower than their roots.
The nerves of the lower spinal segments form a bundle called the cauda equina.
The spinal cord is enlarged in 2 regions: the cervical and lumbosacral areas.
The cervical enlargement innervates the upper extremity at the brachial plexus.
The cervical enlargement includes spinal cord segments from about C4 to T1.
Lumbosacral enlargement corresponds to the lumbosacral plexus nerves, which innervate the lower limb.
Lumbosacral enlargement comprises the spinal cord segments from L2 to S3 and is found about the vertebral levels of T9 to T12.
The floor plate secretes netrins, which act as chemoattractants to decussation of pain and temperature sensory neurons in the alar plate across the anterior white commissure, where they then ascend towards the thalamus.
The central canal of the caudal spinal cord is filled with cerebrospinal fluid.
It is supplied with blood by three arteries that run along its length starting in the brain.
Many arteries that approach the spinal cord through the sides of the spinal column.
There are 3 longitudinal arteries: the anterior spinal artery, and the right and left posterior spinal arteries.
These arteries travel in the subarachnoid space and send branches into the spinal cord, forming anastamoses via the anterior and posterior segmental medullary arteries, which enter the spinal cord at various points along its length.
The major contribution to the arterial blood supply of the spinal cord below the cervical region comes from the radially arranged posterior and anterior radicular arteries.
Impaired blood flow through radicular arteries, especially during surgical procedures that involve abrupt disruption of blood flow through the aorta for example during aortic aneursym repair, can result in spinal cord infarction and paraplegia.
Spinal cord tracts include the somatosensory organization that is divided into the dorsal column-medial lemniscus tract and the anterolateral system, or ALS.
The dorsal column-medial lemniscus tract is the the touch/proprioception/vibration sensory pathway.
The anterolateral system is the pain/temperature sensory pathway.
Sensory pathways use three different neurons to get information from sensory receptors at the periphery to the cerebral cortex, an are designated primary, secondary and tertiary sensory neurons.
Both sensory pathways primary sensory neuron cell bodies are found in the dorsal root ganglia, and their central axons project into the spinal cord.
In the dorsal column-medial leminiscus tract, a primary axon that enters below spinal level T6, the axon travels in the fasciculus gracilis, the medial part of the column.
If the axon enters above level T6, then it travels in the fasciculus cuneatus, which is lateral to the fasciculus gracilis in the dorsal column-medial leminiscus tract.
The primary axon ascends to the lower medulla, where it leaves its fasciculus and synapses with a secondary neuron in one of the dorsal column nuclei: either the nucleus gracilis or the nucleus cuneatus
Subsequently, the secondary axon leaves its nucleus and passes anteriorly and medially, as internal arcuate fibers.
Proprioception of the lower limbs differs from the upper limbs and upper trunk.
Lower limb proprioception involves a four-neuron pathway, which initially follows the dorsal spino-cerebellar pathway.
The anterolateral primary neuron axons enter the spinal cord and then ascend one to two levels before synapsing in the substantia gelatinosa.
The tract that ascends before synapsing is known as Lissauer’s tract.
After synapsing, secondary axons decussate and ascend in the anterior lateral portion of the spinal cord as the spinothalamic tract.
The spinothalamic tract ascends to synapse on tertiary neurons, which then travel to the primary sensory cortex via the posterior limb of the internal capsule.
Actions of the spinal nerves:
Level Motor Function
C1–C6 Neck flexors
C1–T1 Neck extensors
C3, C4, C5 Supply diaphragm (mostly C4)
C5, C6 Move shoulder, raise arm (deltoid); flex elbow (biceps)
C6 externally rotate (supinate) the arm C6, C7 Extend elbow and wrist (triceps and wrist extensors); pronate wrist
C7, C8 Flex wrist; supply small muscles of the hand
T1–T6 Intercostals and trunk above the waist
T7–L1 Abdominal muscles
L1–L4 Flex thigh
L2, L3, L4 Adduct thigh; Extend leg at the knee (quadriceps femoris)
L4, L5, S1 abduct thigh; Flex leg at the knee (hamstrings); Dorsiflex foot (tibialis anterior); Extend toes
L5, S1, S2 Extend leg at the hip (gluteus maximus); Plantar flex foot and flex toes
The corticospinal tract serves as the motor pathway for upper motor neuronal signals coming from the cerebral cortex and from primitive brainstem motor nuclei.
Cortical upper motor neurons originate from Brodmann areas 1, 2, 3, 4, and 6 and then descend in the posterior limb of the internal capsule, through the crus cerebri, down through the pons, and to the medullary pyramids, where about 90% of the axons cross to the contralateral side at the decussation of the pyramids.
They then descend as the lateral corticospinal tract.
These axons synapse with lower motor neurons in the ventral horns of all levels of the spinal cord.
The remaining 10% of axons descend on the ipsilateral side as the ventral corticospinal tract.
These axons also synapse with lower motor neurons in the ventral horns.
Most cross to the contralateral side of the cord right before synapsing.
The midbrain nuclei include four motor tracts that send upper motor neuronal axons down the spinal cord to lower motor neurons: rubrospinal tract, the vestibulospinal tract, the tectospinal tract and the reticulospinal tract.
The function of lower motor neurons can be divided into two different groups: the lateral corticospinal tract and the anterior cortical spinal tract.
The lateral tract contains upper motor neuronal axons which synapse on dorsal lateral lower motor neurons.
The dorsal lateral lower motor neurons. are involved in distal limb control, and are found specifically only in the cervical and lumbosacral enlargements within the spinal cord.
There is no decussation in the lateral corticospinal tract after the decussation at the medullary pyramids.
The anterior corticospinal tract descends ipsilaterally in the anterior column, where the axons emerge and either synapse on lower ventromedial motor neurons in the ventral horn ipsilaterally or descussate at the anterior white commissure where they synapse on ventromedial lower motor neurons contralaterally .
The tectospinal, vestibulospinal and reticulospinal descend ipsilaterally in the anterior column.
Spinocerebellar tracts with proprioceptive information travels up the spinal cord via three tracts: those below L2, from L2 to T1 and above T1.
The proprioceptive information travels up the spinal cord in the ventral spinocerebellar tract below L2.
The ventral spinocerebellar tract sensory receptors take in the information and travel into the spinal cord.
The cell bodies of these primary neurons are located in the dorsal root ganglia.
The cell body axons of primary neurons in the dorsal root ganglion the synapse in the spinal cord, and the secondary neuronal axons decussates and then travel up to the superior cerebellar peduncle where they decussate again, bringing information to deep nuclei of the cerebellum.
At the levels of L2 to T1, proprioceptive information enters the spinal cord and ascends ipsilaterally, where it synapses in Clarke’s nucleus.
The secondary neuronal axons continue to ascend ipsilaterally and then pass into the cerebellum via the inferior cerebellar peduncle (dorsal spinocerebellar tract).
Above T1, proprioceptive primary axons enter the spinal cord and ascend ipsilaterally until reaching the accessory cuneate nucleus, where they synapse. The secondary axons pass into the cerebellum via the inferior cerebellar peduncle where again, these axons synapse on cerebellar deep nuclei.
Motor information travels from the brain down the spinal cord via descending spinal cord tracts.
Descending tracts involve two neurons: the upper motor neuron and lower motor neuron.
A nerve signal travels down the upper motor neuron until it synapses with the lower motor neuron in the spinal cord.
The lower motor neuron conducts the nerve signal to the spinal root where efferent nerve fibers carry the motor signal toward the target muscle.
The descending tracts are composed of white matter.
The lateral and anterior corticospinal tracts are responsible for coordinated limb movements.
Spinal cord injuries can be caused by
Trauma to the spinal column include: stretching, bruising, pressure, severing, punctured and laceration.
The vertebral bones can shatter, causing the spinal cord to be punctured by a sharp fragment of bone.
Victims of spinal cord injuries will suffer loss of feeling in certain parts of their body, and with severe injuries may result in paraplegia, quadriplegia or full body paralysis below the site of injury to the spinal cord.
Upper motor neuron damage to axons in the spinal cord results in a characteristic pattern of ipsilateral deficits.
Upper motor neuron injury findings include hyp2242eflexia, hypertonia and muscle weakness.
Lower motor neuronal damage results in characteristic pattern of deficits, relating to the myotome affected by the damage.
Lower motor neuron injury is characterized by muscle weakness, hypotonia, hyporeflexia and muscle atrophy.
Spinal shock after injury is usually temporary, lasting only for 24–48 hours, and is a temporary absence of sensory and motor functions.
Neurogenic shock that occurs from a spinal injury. can lasts for weeks and can lead to a loss of muscle tone due to disuse of the muscles below the injured site.
The spinal cord is most commonly injured at the cervical spine (C1-C7) and the lumbar spine (L1-L5).
Spinal cord injury can be due to non-traumatic causes such as disease: transverse myelitis, polio, spina bifida, Friedreich’s ataxia, spinal cord tumor, and spinal stenosis.
10,000-12,000 people become paralyzed annually as a result of various injuries to the spinal cord.
Real or suspected spinal cord injuries need immediate immobilization of the spine and head.
Neuroimaging are necessary to define the injuries.
Treatment is aimed on limiting post-injury cell death, promoting cell regeneration, and replacing lost cells.
Regeneration is enhanced by maintaining electric transmission in neural elements.
Replacement of lost cells is being tested by transplants with embryonic stem cells, stem cells from the spinal cord, and spinal cord cells from fetuses.
