Sphincter of Oddi dysfunction is divided into three types: type I consists of patients with a dilated bile duct and abnormal liver functions, type II involves one of those criteria but not both, and type III have none of those criteria.
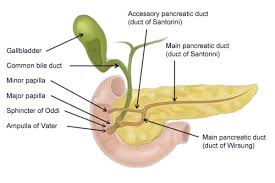
The sphincter of Oddi is a sphincter muscle, a circular band of muscle at the bottom of the biliary tree which controls the flow of pancreatic juices and bile into the second part of the duodenum.
Sphincter of Oddi dysfunction refers to a group of functional disorders leading to abdominal pain due to dysfunction of the Sphincter of Oddi.
The pathogenesis includes stenosis or dyskinesia of the sphincter of Oddi, consequently the terms biliary dyskinesia, papillary stenosis, and postcholecystectomy syndrome have all been used to describe this condition.
Stenosis and dyskinesia can obstruct flow through the sphincter and can cause retention of bile in the biliary tree and pancreatic juice in the pancreatic duct.
Patients present with abdominal pain resembling that of structural or inflammatory disorders of the gallbladder, biliary tree or pancreas.
The pain is typically in the upper part of the abdomen or in the right upper quadrant of the abdomen, lasts 30 minutes or longer, and is not associated with a structural abnormality that could lead to these symptoms.
Classified into two subtypes: functional biliary sphincter of Oddi disorder, where there is no disturbance in pancreatic enzyme measurements, such as amylase and lipase; and, functional pancreatic sphincter of Oddi disorder, where pancreatic enzyme measurements are elevated.
Risk factors include: biliary-pancreatic disease.
Attacks can be precipitated by opioid analgesics,
Opioid analgesics can cause attacks in patients having undergone cholecystectomy or bariatric surgery.
Functional disorders of the gallbladder, bile duct and pancreas have been defined and classified by the Rome criteria for functional gastrointestinal disorders.
The criteria outline three variants of functional disorders of the gallbladder, bile duct and pancreas: the pain must be located in the upper part of the abdomen and/or the right upper quadrant of the abdomen.
episodes of pain must last at least 30 minutes.
the symptoms must be recurrent, and occur at differing intervals.
the pain must incrementally increase to a steady level.
the pain must be severe enough the patient’s daily activities are affected.
the pain must not be relieved by any of bowel movements, change in posture, or antacids.
other structural disorders that could explain the symptoms must be excluded.
If all of the above criteria are met, if the gallbladder is present, and if the testing of liver enzymes, conjugated bilirubin, and pancreatic enzymes are normal, the diagnosis of functional gallbladder disorder is made.
If all of the above criteria are met, individuals are classified as having a functional biliary sphincter of Oddi disorder, if the testing of pancreatic enzymes is normal.
The Milwaukee classification of biliary sphincter of Oddi dysfunction (SOD) divides the condition into three subtypes:
Type I biliary SOD: biliary-type abdominal pain, with all of altered liver enzymes on blood testing, dilated biliary ducts on ultrasound or ERCP, and delayed bile clearance on HIDA scan.
Type II biliary SOD: biliary-type abdominal pain associated with one or two of the following: altered liver enzymes on blood testing, dilated biliary ducts on imaging tests, and delayed bile clearance on HIDA scan.
Type III biliary SOD: biliary-type abdominal pain with none of the following: altered liver enzymes on blood testing, dilated biliary ducts on imaging tests, and delayed bile clearance on HIDA scan.
Individuals are classified as having a functional pancreatic sphincter of Oddi disorder if the above criteria are met, and if the testing of pancreatic enzymes is abnormal.
Sphincter of Oddi dysfunction suggested by pain which seems to come from a biliary origin, which may or may not be associated with transient increases of liver or pancreatic enzymes.
Common bile duct dilation and episodes of pancreatitis are also signs.
Two mechanisms are involved in the development of sphincter of Oddi dysfunction: stenosis, or narrowing of the sphincter of Oddi and dyskinesia, or alteration in the function of the sphincter of Oddi.
With stenosis of the sphincter of Oddi typically have an elevated baseline pressure of the sphincter of Oddi, due to narrowing of the sphincter, such as recurrent passage of gallstones through the ampulla of Vater, trauma to the sphincter from procedures such as endoscopic retrograde cholangiopancreatography or biliary surgery, or infections of the common bile duct.
Dyskinesia of the sphincter of Oddi is a purely functional disorder, wherein there is intermittent obstruction of the bile duct due to inappropriate spasms.
Dyskinesia of the sphincter of Oddi is believed to be due to alteration in local gut hormones and peptides, such as cholecystokinin, which act on the sphincter or to altered neuronal control of the sphincter.
For diagnosis : measurement of liver biochemistry and pancreatic enzymes, ruling out structural abnormalities, by abdominal ultrasound and endoscopic retrograde cholangiopancreatography (ERCP).
Best diagnosed using manometry-an internal test done to measure the pressures within surrounding ducts to determine whether or not the muscle is functioning normally.
Medication to prevent spasms or sphincterotomy are the standard treatments for sphincter of Oddi dysfunction.
