 Small cell lung cancer accounts for approximately 18-25% of lung cancer worldwide.
Small cell lung cancer accounts for approximately 18-25% of lung cancer worldwide.
Accounts for about 15% of lung cancers diagnosed in the U.S.
Prevalence is decreasing due to decreases in smoking.
The most aggressive form of lung cancer characterized by rapid responses to chemotherapy and sensitivity to radiotherapy and due to early treatment resistance, the five-year survival is less than 10%.
Approximately 66% of patients have metastasis at the initial diagnosis.
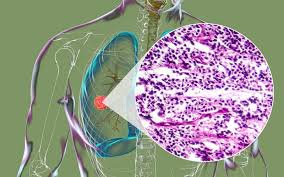
Categorized as high grade neuroendocrine carcinoma.
Its mitotic rate is high compared with atypical and typical carcinoids.
SCLC neuroendocrine cancer is associated with paraneoplastic syndromes and is characterized by rapid proliferation index, a high growth fraction, and early metastases.
For untreated patients, the median overall survival from diagnosis is approximately 2 to 4 months and with treatment the median overall survival is 16 to 24 months for patients with limited stage SCLC but only 6 to 12 months for those with extensive stage SCLC.
Up to 30% of specimens from patients with SCLC reveal NSCLC differentiation suggesting pulmonary carcinogenesis is from a pleural potential stem cell.
Neuroendocrine tumors account for approximately 20% of lung cancers most of the which (14%) is small cell lung cancer.
Approximately 33,000 new cases in the US annually.
Characterized by rapid doubling time and early, widespread metastases, and is the most aggressive form of lung cancer.
Incidence has been decreasing in the U.S. for the last several years.
Incidence decreasing over the past 30 years, presumably because of the decrease in the number of smokers and change to low-tar filter cigarettes.
SCLC in light/never smokers, is very rare and comprises fewer than 2.5% of cases.
Light or never smokers, are more likely to be female, to be with an age group 35 to 49 years or greater than 80 years of age, and to present with an extensive stage.
Light or never smokers, have a lower tumor mutational burden, lower frequency of TP53 mutations, and a higher frequency of EGFR and SMAD4 mutations.
There is no overall survival differences between light/never smokers or smokers in SCLC.
Incidence in women increasing and the male:female incidence now 1:1.
Decrease in incidence related to decreased percentage of smokers and change in cigarette composition.
More than 90% of patients with SCLC are current or past smokers and risk is related to duration and degree of smoking.
Associated more than any other cancer with exposure to Tobacco carcinogens.
Lung cancer screening with CT scans does not improve survival.
The histologic transformation of SCLC from NSCLC is becoming more frequent, with incidence of up to 15%.
The mechanism of histologic transformation is acquired resistance to chemotherapy/radiation, and targeted therapies.
Continued smoking associated with increased toxicity during treatment and shorter survival.
Small cell lung cancer characterized by initial sensitivity to chemotherapy followed by progression and resistant disease.
Rapid doubling time, high growth fraction early development of widespread disease distinguish small cell cancer of the lung from non-small cell lung cancer.
At presentation approximately one-third have limited-stage disease and two-thirds have extensive-stage disease.
Prognosis for patients with extensive stage SCLC is particularly poor, with the two-year survival rate of less than 5% typically reported with platinum-doublet chemotherapy regimens.
Poor prognostic features include: impaired performance status, weight loss, increased stage, male sex, elevated LDH and low sodium due to syndrome of inappropriate ADH.
Second line treatment for small cell lung cancer options remain limited, with a short duration of response, ranging from 3.6 to 5.3 months, and an overall survival that rarely exceeds eight months.
A higher total gross tumor volume predicts the worse outcome in patients with local advanced small cell lung cancer.
Patients typically present with a hilar mass and bulky mediastinal lymphadenopathy that causes cough and dyspnea.
Frequently present with symptoms of widespread metastatic disease, such as weight loss, debility, bone pain, and neurologic compromise.
Limited stage disease is defined as stage I-IIIB using the TMN disease.
Limited stage disease is defined as tumor confined to one hemithorax and can be encompassed within 1 radiation field.
The addition of thoracic radiation therapy to chemotherapy has improved survival for patients with limited stage disease: revealing a 14% reduction in the mortality rate and an absolute 5.4% difference in the three year survival rate when compared to chemotherapy alone.
Adjuvant radiation/chemo therapy versus chemo therapy alone in limited disease improves local control by more than 25%, but long-term control remains limited.
Approximately one third of patients present with limited disease with a 5 year survival rate of 13-38%.
Five-year survival for extensive disease patients is only 7%.
There two main drivers of small cell lung cancer are loss-of-function mutations in 2 key tumor suppressor genes TP53 and RB1.
TP 53 inactivation in approximately 75 to 90% of small cell lung cancers, and RB1 in approximately 69 to 90% of tumors.
It is held the complete genomic loss of TP53 and RB1 is obligatory in SCLC.
United Kingdom Medical Research Council reported randomized study of surgical resection vs thoracic radiation: 5-year survival 1% with surgery and 4% with thoracic surgery, and 10 year survival 0% and 4%, respectively.
Surgery is appropriately only for a few patients, about 2-5% woth surgically resectable disease stage I.
Staging evaluation is recommended with diagnosis and consists of a medical history, physical examination, complete blood count, chemistry panel, CT scan of the chest and abdomen with intravenous contrast, CT scan of the chest extending to the liver and adrenal glands, magnetic resonance imaging and bone scan (If PET scan is obtained bone scan can be omitted).
PET scans can increase staging accuracy in patients with SCLC with approximately 19 patients having upstage disease and 8% down staged from extensive to limited stage disease.
A bone marrow aspirate and biopsy may be indicated in patients with nucleated red blood cells, neutropenia, or thrombocytopenia suggestive of bone marrow infiltration: bone marrow involvement is the only side if extensive stage disease occurs in fewer than 5% of patients.
It is recommended did both LS (limited stage) versus ES (extensive stage) and the TNM classification be used for staging.
In patients with clinical stage I disease being considered for curative surgical resection, invasive mediastinal staging and extrathoracic imaging is recommended.
In patients with clinical stage I disease, if the evaluation for distant metastases and invasive mediastinal stage evaluation is negative, surgical resection is suggested over non-surgical treatment.
In patients with stage I SCLC who have undergone curative intent surgical resection, platinum based adjuvant chemotherapy is recommended.
All patients with small cell lung cancer requires systemic therapy either as primary or adjument therapy.
In patients with limited stage SCLC early chemoradiotherapy with accelerated type of fractionated radiation therapy concurrently with platinum days chemotherapy is recommended.
In patients with limited stage or extensive Stege SCLC who achieve a complete or partial response to initial therapy prophylactic cranial radiation is recommended.
Because patients with limited stage disease have potential for cure, prophylactic cranial radiation remains a recommendation for those without high risk factors for the development of cognitive dysfunction.
In patients with extensive SCLC who have completed chemotherapy and achieve a complete response outside the chest and a complete or partial response in the chest, a course of consolidated thoracic radiation is suggested.
In a randomized study of patients responding to chemotherapy with cyclophosphamise, doxorubicin, and vincristine and than randomized to surgical resection and radiation or radiation alone: no improvement in survival noted with the addition of surgery to induction chemotherapy and radiation (Lad T et al).
Bcl-2 frequently overexpressed in small cell lung cancer, and its up regulation has been seen with chemotherapy resistance.
Positive immunohistochemistry for chromogranin Synaptophysin,CD 56 ,and on occasion non specific enolase and keratin.
Nearly all SCLC‘s are immunoreactive for cytokeritan, 85 to 90% are positive for thyroid transcription factor –1.
Napsin A, a marker for adenocarcinoma and P40 is a marker for squamous cell carcinoma, are generally negative in SCLC.
High serum levels of VEGF correlate with chemotherapy resistnce and poor survival in SCLC.
Prognostic factors include: stage, performance status, weight loss as the most reproducible factors.
10% have brain metastases at the time of diagnosis and 40% will develop symptomatic brain metastases.
The incidence of brain metastases as the first site of failure is 15-45% in small cell cancer of the lung.
survival outcomes are equitable following treatment with stereotactic radiosurgery compared with whole brain radiation in patients with small cell lung cancer and brain metastasis.
There are many neurologic and endocrine paraneoplastic syndromes associated with SCLC including Lambert-Eaton myasthenic syndrome, encephalomyelitis, and sensory neuropathy.
Patients with SLCL sometimes produce poly peptide hormones including vasopressin, ADH, and ACTH, which cause hyponatremia of malignancy with the syndrome of inappropriate ADH, and Cushing, respectively.
Some patients with small cell cancer have direct voltage gated calcium channels antibodies, and antibodies that cross react with small cell carcinoma antigens and human neuronal RNA binding proteins resulting in multiple neurological deficits.
Without treatment a median survival of 2-4 months.
For limited disease a median survival 16-24 months with current chemotherapy regimens.
5 year survival rates of approximately 40-60% for patients undergoing surgery for stage I disease.
Surgery with adjuvant chemotherapy is now recommended for the treatment of patients with clinical stage TI-T2 N0 M0 SCLC.
Median survival of only 6-10 months for currently available treatments.
Only about 10% of patients remain free of disease 2 years from the start of therapy, and 5-10% survive for 5 years.
In patients with limited disease and good performance status 5-year survival rate with aggressive management approaches 26%.
In patients with limited disease the goal of treatment is cure with chemotherapy and radiation therapy.
In patients with limited disease, bone marrow aspiration biopsy are advised in the case of abnormal blood counts.
Surgery appropriate for only 2-5% of patients, with stage I resectable disease.
The currently available randomized trials do not support a role for surgical resection in the management of stage I to III SCLC.
Highly sensitive to intial chemotherapy and radiotherapy, however most die of recurrent disease.
Rarely associated with hypercalcemia, but its presence suggests extensive bone and bone marrow involvement.
40% of patients may have a positive bone scan at the time of diagnosis.
Prophylactic brain radiation appears to benefit those who receive complete or near complete remission from chemotherapy.
Chemotherapy remains primary modality of therapy because the majority of patients have occult metastatic disease.
Use of high dose chemotherapy with stem cell or bone marrow transplant does not lead to improvement in survival and increasing the number of cycles of chemotherapy beyond 4-6 also does not result in advantages.
NCCN Guidelines in 2020 suggest the preferred regimens as carboplatin, etoposide, and Atezolizumab, followed by Atezolizumab maintenance: other options include carboplatinum or cis-platinum with etoposide and durvalumab, followed by durvalumab maintenance.
Etoposide and cisplatin associated with an overall and complete response rate of 60-80% and 10-20%, respectively, with a median survival of 8-10 months and 1-2 year survival rates of 30-40% and 5-10%, respectively.
Etoposide and cisplatin superior to cyclophosphamide, epirubicin, and vincristine with significantly higher 2 and 5 year survival rates (14 and 5% and 6 and 2%, respectively (Sundstrom S).
Carboplatin has comparable efficacy and less toxicity than cisplatin.
Platinum with etoposide or irinotecan standard treatments.
Prophylactic cranial radiation demonstrates a 5.4% improvement in 3-year survival (20.7% vs 15.3%) with an absolute reduction in the cumulative incidence of brain metastases at 3 years from 58.6% to 33.3% compared to a control group.
Prophylactic cranial irradiation reduces the risk of brain metastases and improves survival compared with controls, but studies include mainly patients with limited stage disease.
For patients receiving prophylactic cranial irradiation with extensive stage disease fewer patients had symptomatic brain metastases (15% versus 40% at one year) and a longer overall survival (27% versus 13% at 1 year compared with patients who received no further therapy.
Early concurrent chemoradiation yields superior survival results compared with delayed or sequential radiotherapy.
There is a small improvement in the two year overall survival for early thoracic radiation versus late thoracic radiation in limited stage disease.
Meta analyses show that radiation added to chemotherapy decreases thoracic recurrence rate.
Thoracic radiation an integral part of treatment of localized disease controversy exists in its dose, fractionation and timing.
Currently no predictive biomarker is available and program death ligand-1 and mutational burden testing are not recommended in routine practice.
For all patients with small cell lung cancer, systemic therapy’s essential component of treatment.
For all patients with small cell lung cancer, systemic therapy is essential component of treatment.
Many single chemotherapy agents and combination regimens are active in SCLC.
For patients with extensive stage disease systemic therapy alone is recommended.
Efficacious agents include cisplatinum/carboplatinum based therapy.
Platinum based therapy with etoposide, or irinotecan chemotherapy remain the standard first line treatment for extensive stage SCLC a median overall survival of 9 to 11 months.
Irinotecan among the most active agents with a response rate of 37% as a single agent.
Irinotecan and cisplatin response rate 84% with 9% complete remission rate and a median survival of 12.8 months.
For patients who relapse more than 6 months after the end of initial treatment, retreatment with the same agents should be considered.
Chemotherapy generally results in a median progression free survival of 2-6 months and a median overal survival of 9-10 months.
Findings of a phase 1/II CheckMate 032 study showed an overall response rate of 46% with a combination of nivolumab and ipilimumab.
Chemotherapy plus immunotherapy is now approved for patients with extensive small cell lung cancer.
Nivolumab first checkpoint inhibitor approval was based on efficacy and safety data from the phase 1/2 CheckMate-032 trial: 109 patients received nivolumab after platinum-based chemotherapy and at least one other prior line of therapy, and 12% responded
Checkpoint inhibitors have emerged as a standard first line treatment for many tumor types and in SCLC they are associated with a longer overall survival.
CheckMate 331 A phase III trial comparing Nivolumab to chemotherapy in patients with metastatic small cell lung cancer who progressed after first line platinum-based chemotherapy: overall survival with Nivolumab was 79% at 15.8 months and 86% with secondary chemotherapy.
Topotecan second-line therapy is the only therapy approved by the FDA, but other Agents commonly used include irinotecan, paclitaxel, docetaxel, temozolomide, vinorelbine, nivolumab, ipilimumab, etopodide, gemcitabine, cyclophosphamide/doxorubicin/vincristine, bendamustine.
FDA granted accelerated approval to pembrolizumab for the treatment of patients who have metastatic small cell lung cancer (SCLC) that progresses on or after platinum-based chemotherapy and at least one other line of therapy.
Pembrolizumab response rate was 19% with 2% complete remission rate, with duration of response of greater than six months in 94%, greater than 12 months in 63% and greater than 18 months in 56%.
The FDA has granted an approval to the combination of atezolizumab (Tecentriq) with carboplatin and etoposide for the frontline treatment of patients with extensive-stage small cell lung cancer (ES-SCLC).
Phase III IMpower133 study, which demonstrated that the addition of atezolizumab to carboplatin and etoposide led to a significant improvement in overall survival (OS) in patients with ES-SCLC.
The median OS in IMpower133 was 12.3 months in the atezolizumab arm compared with 10.3 months in the carboplatin/etoposide and placebo arm, leading to a 30% reduction in the risk of death.
The median progression-free survival (PFS) was 5.2 months in the atezolizumab arm compared with 4.3 months in the placebo group.
There was no major difference in ORR between arms (60.2% vs 64.4%) or in median duration of response (4.2 vs 3.9 months).
Atezolizumab was associated with a higher 6-month PFS rate (30.9% vs. 22.4%), and a more than doubling 12-month PFS rate (12.6% vs 5.4%) compared with placebo.
It demonstrated superior 6-month (32.2% vs 17.1%) and 12-month (14.9% vs 6.2%) event-free rates.
The FDA approved pembrolizumab as a treatment option for patients with metastatic small-cell lung cancer.
The clinical response rates from KEYNOTE-158 and KEYNOTE-028,
showed disease progression on or after platinum-based chemotherapy and at least one other prior line of therapy.
The overall response rate was 19%, and the complete response rate was 2%.
Responses were durable for 6 months or longer in 94%, 12 months or longer in 63%, and 18 months or longer in 56% of the 16 responding patients.
Responses were durable for 6 months or longer in 94%, 12 months or longer in 63%, and 18 months or longer in 56% of the 16 responding patients.
CASPIAN trial showed the combination of durvalumab and etoposide achieved significant improvement in overall survival compared to etoposide alone.
Phase 3 CASPIAN trial showed maintained overall survival (OS) benefit of durvalumab treatment in combination with platinum etoposide chemotherapy vs chemotherapy alone, in newly diagnosed patients with extensive-stage small cell lung cancer (ES-SCLC) after more than 2 years of follow-up.
More than 10% of patients on durvalumab plus chemotherapy had not progressed and remained on treatment at two years vs 2.9% on chemotherapy alone.
The FDA has approved durvalumab (Imfinzi) for the first-line treatment of adult patients with extensive-stage small cell lung cancer (ES-SCLC) for use in combination with standard-of-care chemotherapy, including etoposide plus either carboplatin or cisplatin.
Durvalumab plus platinum-etoposise is presently a new standard of care for first line treatment of extensive stage small cell lung carcinoma.
Durvalumab after chemoradiotherapy, adjuvant therapy leads to significant longer overall survival and progression free survival than placebo among patients with limited stage small cell lung cancer (Cheng Y
It is approved by the FDA for the treatment of patients with locally advanced, unresectable stage III non–small cell lung cancer who have not progressed following chemoradiotherapy.
((Lurbinectedin)), a novel selective inhibitor of oncogenic transcription, had encouraging activity when given as second-line therapy in patients with relapsed small-cell lung cancer (SCLC).
CAPSTONE1 trial show day adding adebrelimab, a PD-L1 antibody to chemotherapy significantly improves overall survival with an acceptable safety profile in patients with extensive stage SCLC.
Serplulimab is a fully humanized IgG4 monoclonal antibody against the PD-1 receptor: in a trial of previously untreated extensive stage SCLC serplulimab plus chemotherapy significantly improved overall survival compared with chemotherapy alone open (Chang Y).
Tarlatamab a bispecific T cell, engager immunotherapy that directs the patients T cells to cancer cells that express a delta like ligand 3 showed anti turmeric activity with durable objective responses and promising survival outcomes in patients with previously treated small cell lung cancer (Ahn MJ).
In the EXTENTORCH trial it was found that adding the anti—PD-1 antibody topalimab to platinum plus etoposide with early stage small cell lung cancer significantly improved both progressive free survival and overall survival.
Presently a combination of etoposide and platinum doublet chemotherapy with an anti-program death ligand-1 (PDL-1) directed therapy has become the Standard Of Care Frontline for early stage small cell lung cancer.
Overall survival was prolonged for approximately two months when PD-L1 inhibitors were added to chemotherapy compared to chemotherapy alone.
