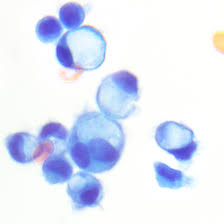
 Signet ring cell defined as a malignant cell with a large intracytoplasmic vacuole appearing as a crescent causing a peripheral displacement of the nucleus.
Signet ring cell defined as a malignant cell with a large intracytoplasmic vacuole appearing as a crescent causing a peripheral displacement of the nucleus.
Signet ring cell carcinoma (SRCC) is a rare form of highly malignant adenocarcinoma that produces mucin.
It is an epithelial malignancy characterized by the histologic appearance of signet ring cells.
Commonly begin in the stomach, colon, pancreas, urinary bladder, thyroid and rarely in the prostate.
Primary SRCC tumors are most often found in the glandular cells of the stomach.
Signet ring cell carcinoma originates in the stomach in 56 percent of patients, and less frequently in the breast, gallbladder, urinary bladder, and pancreas.
Though incidence and mortality of gastric cancer has declined in many countries over the past 50 years, there has been an increase in occurrences of gastric SRCC-type cancers.
Such tumors grow in characteristic sheets, which makes diagnosis using standard imaging techniques, like CT and PET scans, less effective.
Some cases are inherited, and these cases are often caused by mutations in the CDH1 gene, which encodes the celiac cell adhesion glycoprotein E-cadherin.
SRCCs are dedifferentiated adenocarcinomas that lose the capability for celiac cell interaction.
Highly differentiated adenocarcinomas form signet ring cell carcinoma via a loss of adherence and tight junctions that typically separate MUC4, a mucin protein, and ErbB2, an oncogenic receptor.
When MUC4 and ErbB2 interact, they trigger an activation loop, resulting in ErbB2/ErbB3 signaling pathway becomes constitutively activated, and celiac cell interactions are lost and signet carcinomas are formed.
The action of the ErbB2/ErbB3 complex also enhances cell growth.
The pattern of metastasis is different for gastric signet cell carcinoma than for intestinal-type gastric carcinoma.
Somatic mutations of the APC gene have also been implicated in the development of gastric SRCCs.
Stomach cancers with both adenocarcinoma and some SRCexhibit more aggressive behavior than purely SRCC or non-SRCC histologies.
They do not normally form in the lungs, though a few incidences have been reported.
Cases of gastric carcinomas metastasizing to the breast and forming signet-ring cells have also been reported.
In advanced gastric cancers, the prognosis for patients with the SRCCs was significantly worse than for the other histological types.
Advanced SRCC gastric cancers have a larger tumor size, more lymph node metastasis, a deeper invasive depth and more Borrmann type 4 lesions than other types.
SRCC in the stomach occurs more often in women and younger patients.
Patients with SRCC of the stomach show similar clinicopathological features to patients with undifferentiated histology.
SRCC tumors often are seen in the peritoneum and has lymphatic permeation to the lungs and to the ovaries, creating Krukenberg tumors.
Of the prostate occurs in 1% of adenocarcinomas of the prostate.
Should be classified as a high grade adenocarcinoma when it involves the prostate.
Signet cell carcinoma of the prostate presents with delayed symptoms and more than 40% of patients present with advanced disease.
Survival rates for signet cell cancer of the prostate is poor because of late diagnosis with advanced stage disease and, with 3 year survival of 55% and 5 year survivals of 12%.
Establishing a diagnosis of signet cell carcinoma of the prostate requires histopathological examination of prostate tissue, and negative gastrointestinal workup and stains to help localize the primary site of the cancer to the prostate.
The average age at diagnosis of signet cell carcinoma of the prostate is 68 years, with a mean survival of 29 months.
75% of cases or locally advanced or metastatic at the time of diagnosis.
Signet cell prostate cancer usually stains negative for CEA, but may be positive in 20% of cases.
Signet cell carcinoma of the prostate usually stains positive for PSA.
Signet cell carcinoma of the prostate cytoplasmic vacuoles contain lipid or mucin and stains positive for mucicarmine in about 50% of cases, and PAS positive in 60% of cases and positive for alcian blue in 60% of cases.
Among colorectal cancers, the prevalence of SRCC is less than one percent.
Signet cells resemble signet rings, which result from the formation of large vacuoles full of mucin that displace the nucleus to the cell’s periphery.
A study of SRCC colorectal cancers compared mucin-rich SRCC tumors and mucin-poor SRCC tumors.
Mucin-poor SRCC colorectal tumors more frequently demonstrated adverse histologic features such as lymphatic invasion, venous invasion and perineural invasion.
Chemotherapy has relatively poor curative efficacy in SRCC patients.
Overall survival rates are lower compared to patients with more typical cancer pathology.
SRCC cancers are usually diagnosed during the late stages of the disease, so the tumors generally spread more aggressively than non-signet cancers, making treatment challenging.
In SRCC of the stomach, removal of the stomach cancer is the treatment of choice.
There is no combination of chemotherapy which is clearly superior to others: but most active agents include 5-Fluorouracil (5-FU), Cisplatin, and/or Etoposide, Taxol and Gemcitabine.
These aggressive tumors are generally diagnosed at advanced stages and survival is generally shorter.
Primary signet-ring cell carcinoma of the urinary bladder is extremely rare and patient survival is very poor and occurs mainly in men ages 38 to 83.
Primary signet ring cell carcinoma of the colon and rectum (PSRCCR) is rare, with a reported incidence of less than 1 percent.
It has a poor prognosis because symptoms often develop late and it is usually diagnosed at an advanced stage.
Five-year survival rates in previous studies ranged from nine to 30 percent.
Average survival was between 20 and 45 months.
It tends to affect younger adults with higher likelihood of lymphovascular invasion.
The overall survival rate of patients with SRCC was significantly poorer than that of patients with mucinous or poorly differentiated adenocarcinoma.
