 Sensory Processing Disorder (SPD) is a condition that affects how the brain processes incoming information from the senses, such as sight, sound, touch, taste, and smell.
Sensory Processing Disorder (SPD) is a condition that affects how the brain processes incoming information from the senses, such as sight, sound, touch, taste, and smell.
People with SPD may overreact or underreact to certain stimuli, and can find certain sensations overwhelming or unbearable.
SPD can affect people of all ages, and is commonly found in individuals with autism spectrum disorders, as well as those with attention deficit hyperactivity disorder (ADHD), anxiety disorders, and other developmental and neurological conditions.
Sensory Processing Disorder (SPD), is also known as Sensory Integration Disorder.
It occurs when the brain has trouble organizing and responding to information received through the senses.
This can include difficulties regulating emotions, behavior, and social interaction.
Some common signs of SPD in children may include being extremely sensitive to touch or sound, avoiding certain foods due to their texture or smell, being bothered by certain fabrics in clothing, or seeking out intense sensations such as spinning or jumping.
Adults with SPD can also experience sensory issues that affect daily life and functioning.
Treatment for SPD often includes occupational therapy, which can help individuals develop skills to regulate their sensory responses and improve their ability to process sensory information.
Additionally, creating a sensory-friendly environment at home or work can help reduce triggers and improve daily functioning.
It’s important to note that SPD can vary greatly between individuals, and diagnosis and treatment plans should always be personalized to meet the specific needs of each person.
Sensory processing disorder (SPD) is a condition in which multisensory input is not adequately processed in order to provide appropriate responses to the demands of the environment.
Sensory processing disorder is present in many people with autism spectrum disorder and attention deficit hyperactivity disorder.
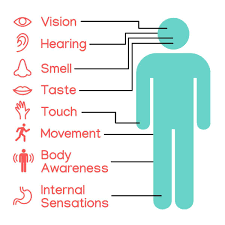
Patients with SPD may inadequately process visual, auditory, olfactory, taste, tactile, vestibular, proprioception and interoception sensory stimuli.
Associated with hypersensitivity and hyposensitivity to stimuli, and/or difficulties using sensory information to plan movement.
Complications of SPD:
Low school performance, behavioral difficulties, social isolation, employment problems, family and personal stress.
Normally the body organizes its sensations and those from the environment and makes it possible to use the body effectively within the environment.
SPD is characterized by difficulties in the performance in one or more of the main areas of life: productivity, leisure and play or activities of daily living.
SPD is not included in Diagnostic and Statistical Manual of Mental Disorders of the American Psychiatric Association.
SPD is characterized by persistent abnormalities with neurological processing of sensory stimuli that interfere with a person’s ability to participate in everyday life.
One or several sensory systems of the somatosensory system, vestibular system, proprioceptive system, interoceptive system, auditory system, visual system, olfactory system, and gustatory system are involved.
Signs of over-responsivity to stimuli include: dislike of textures such as those found in fabrics, foods, grooming products or other materials to which most people would not react, and manifestations of discomfort, sickness or threat induced by normal sounds, lights, ambient temperature, movements, smells, tastes, or even inner sensations such as heartbeat.
Signs of under-responsivity include: sluggishness and lack of responsiveness.
Sensory cravings include: fidgeting, impulsiveness, and/or seeking or making loud, disturbing noises; and sensorimotor-based problems, including slow and uncoordinated movements or poor handwriting.
Sensory discrimination problems, which might manifest themselves as things constantly dropped.
Sensory integration and processing difficulties can be seen in a number of disorders: anxiety problems, attention deficit hyperactivity disorder (ADHD), food intolerances, behavioral disorders, and particularly, autism spectrum disorders.
The midbrain and brainstem regions of the central nervous system are early centers in the processing pathway for multisensory integration; processes include coordination, attention, arousal, and autonomic function.
Sensory information passes through these centers, and is routed to brain regions responsible for emotions, memory, and higher level cognitive functions.
Therefore, damage to any part of the brain involved in multisensory processing can cause difficulties in adequately processing stimuli.
Electroencephalography (EEG), measuring event-related potential (ERP) and magnetoencephalography (MEG) are traditionally used to explore the causes behind the behaviors observed in sensory processing disorder.
Tactile and auditory over-responsivity show moderate genetic influences, with tactile over-responsivity demonstrating greater heritability.
Differences in auditory latency, the time between the input is received and when reaction is observed in the brain: hypersensitivity to vibration in the Pacinian corpuscles receptor pathways and other alterations in unimodal and multisensory processing have been detected in autism populations.
People with sensory processing deficits have atypical neural integration of sensory input.
In people with sensory over-responsivity, different neural generators activate, causing associations of causally related sensory inputs that do not function properly.
Patients with sensory over-responsivity might have increased D2 receptors in the striatum, related to aversion to tactile stimuli.
There is abnormal white matter microstructure in children with SPD, compared with normal children and those with other developmental disorders such as autism and ADHD.
Sensory processing disorder is accepted in the Diagnostic Classification of Mental Health and Developmental Disorders of Infancy and Early Childhood, but is not recognized as a mental disorder in medical manuals such as the ICD-10or the DSM-5.
Diagnosis is primarily arrived at by the use of standardized tests, standardized questionnaires, expert observational scales, and free-play observation at occupational therapy.
Diagnosis is commonly made by an occupational therapist, or by certified professionals, such as psychologists, learning specialists, physiotherapists and/or speech and language therapists.
Standardized tests:
Sensory Integration and Praxis Test (SIPT)
Evaluation of Ayres’ Sensory Integration (EASI)
DeGangi-Berk Test of Sensory Integration
Test of Sensory Functions in Infants (TSFI)
Standardized questionnaires
Sensory Profile (SP)
Infant/Toddler Sensory Profile
Adolescent/Adult Sensory Profile
Sensory Profile School Companion
Indicators of Developmental Risk Signals (INDIPCD-R)
Sensory Processing Measure (SPM)
Sensory Processing Measure Preeschool (SPM-P)
Sensory integration and processing difficulties:
Sensory registration and perception (discrimination)
Sensory reactivity (modulation)
Praxis
Postural, ocular and bilateral integration
Proponents of a new nosology SPD have propose three categories: sensory modulation disorder, sensory-based motor disorders and sensory discrimination disorders.
Sensory modulation disorder (SMD)
refers to a complex central nervous system process by which neural messages that convey information about the intensity, frequency, duration, complexity, and novelty of sensory stimuli are adjusted.
It has three subtypes:
Sensory over-responsivity.
Sensory under-responsivity
Sensory craving/seeking.
Sensory-based motor disorder (SBMD)
Sensory-based motor disorder shows motor output that is disorganized as a result of incorrect processing of sensory information affecting postural control challenges, resulting in postural disorder, or developmental coordination disorder.
The SBMD subtypes are:
Dyspraxia
Postural disorder
Sensory discrimination disorder (SDD)
Sensory discrimination disorder involves the incorrect processing of sensory information.
The SDD subtypes are:
Visual
Auditory
Tactile
Gustatory
Olfactory
Vestibular
Proprioceptive
Interoception
Sensory integration therapy is driven by four main principles:
The child must be able to successfully meet the challenges that are presented through playful activities.
Adaptive response, the child adapts their behavior with new and useful strategies in response to the challenges presented.
Active engagement
Child directed preferences are used to initiate therapeutic experiences within the session.
Sensory processing therapy retains all of the above-mentioned four principles and adds:
Intensity- to attend therapy daily for a prolonged period of time.
Therapist adaptation to the developmental age of the person.
Test-retest evaluations before and after
Happiness of life is therapy’s main goal, attained through social participation, self-regulation, and self-esteem.
Sensory integration therapy effectiveness is unproven,
It has been estimated by proponents that up to 16.5% of elementary school aged children present elevated sensory over responsivity behaviors in the tactile or auditory modalities.
There are concerns regarding the validity of the diagnosis.
SPD is not included in the DSM-5 or ICD-10, the most widely used diagnostic sources in healthcare.
