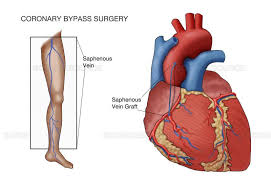
 Saphenous vein grafts (SVG) are the most frequently used conduits in coronary artery bypass graft (CABG) surgery.
Saphenous vein grafts (SVG) are the most frequently used conduits in coronary artery bypass graft (CABG) surgery.
In the United States there is approximately 300,000 patients undergoing CABG surgery annually, and the saphenous vein is used in more than 90% of such procedures.
As many ass 10 to 25% of SVGs occlude within the first year after surgery.
Early saphenous vein graft failure is mainly due to thrombosis subsequent to endothelial damage or endothelial activation that leads to a prothrombotic state.
The use of the left internal mammary artery as a conduit is associated with the highest 10-year patency rate (>90%), saphenous vein grafts, the most commonly used conduit in CABG surgery, fail in 40−50% of treated patients by 10 years after surgery.
Vein graft disease (VGD) and failure result from complex pathophysiological processes may lead to complete occlusion of the graft.
Optimal harvesting techniques, intraoperative preservation strategies and intraoperative patency control have important roles in the prevention of vein graft disease.
Studies published in the past decade have reported similar mid-term patency rates between vein grafts and arterial grafts when veins are used as a composite graft based on the internal mammary artery.
Endothelial damage attributable to mechanical harm and ischemia–reperfusion injury contribute to the development of vein graft damage and failure, mediated by thrombosis, intimal hyperplasia and atherosclerosis in the early, intermediate and late phases, respectively.
To prevent saphenous vein graft dysfunction requires meticulous harvesting strategy to reduce surgical trauma and avoid excessive handling and distention.
Optimizing intraoperative preservation of SVGs to maintain normal endothelial function and integrity during harvesting reduces the occurrence of saphenous vein graft dysfunction.
Intraoperative graft flow assessment is important in identifying grafts that have initial low flow and can provide an opportunity to correct the issue intraoperatively.
The inhibition of platelet aggregation with aspirin after CABG surgery reduces early saphenous vein graft failure and is presently endorsed by current practice guidelines.
Dual antiplatelet therapy with aspirin and an oral platelet P2Y12 receptor inhibitor is associated with enhanced platelet inhibitory effects.
In 4 randomized clinical trials of patients undergoing coronary artery bypass graft surgery, the addition of ticagrelor to aspirin was associated with a significantly decreased risk of vein graft failure, as well as a significant increase risk of clinically important bleeding.
