

 Usually located on pressure points in patients with rheumatoid arthritis.
Usually located on pressure points in patients with rheumatoid arthritis.
A rheumatoid nodule is an area of swelling, that appears on the exterior of the skin usually around the olecranon (or the interphalangeal joints but can appear in other areas.
There are four different types of rheumatoid nodules: subcutaneous rheumatoid nodules, cardiac nodules, pulmonary nodules, and central nervous systems nodules.
These nodules occur almost exclusively in association with rheumatoid arthritis.
Very rarely do rheumatoid nodules occur in the absence of rheumatoid arthritis.
Rheumatoid nodules can also appear in areas of the body other than the skin.
Less commonly they are found in the lining of the lungs or other internal organs.
The occurrence of nodules in the lungs of miners exposed to silica dust is. known as Caplan’s syndrome.
Rarely, nodules can occur at diverse sites on body: upper eyelid, distal region of the soles of the feet, vulva, and internally in the gallbladder, lung, heart valves, larynx, and spine.
Rheumatoid nodule histlologically has characteristic palisading granuloma with a core consisting of necrotic collagen and fibrin.
The pathology is characterized by central necrosis, palisading mononuclear cells, and perivascular lymphocytic infiltrations.
Rheumatoid nodules can vary in size from 2 mm to 5 cm and are usually rather firm.
Often rheumatoid nodules are associated with synovial pockets or bursae.
About 5% of people with rheumatoid arthritis have such nodules within two years of disease onset, and the cumulative prevalence is about 20–30%.
Risk factors of developing rheumatoid nodules include smoking and trauma to small vessels.
The majority of nodules are not painful or disabling in any way.
They are usually more of an unsightly nuisance.
Rheumatoid nodules can become painful when infection or ulcers occur on the skin of the nodule.
Nodules may disappear or grow larger over time, making nodular size difficult to predict.
Treatment of rheumatoid nodules can be difficult: surgical removal and injection of corticosteroids have shown good results.
Rheumatoid nodules frequently form over extensor sites and areas vulnerable to trauma.
Such trauma can cause inflammatory particles to build up and lead to a secondary inflammatory response which ultimately causes fibrin release and necrosis.
It is suggested that the inflammation of blood vessels activates complement components, which leads to the deposit of rheumatoid factors and fibrin.
The rheumatoid nodule is the most common cutaneous manifestation of rheumatoid arthritis.
Rheumatoid arthritis involves chronic inflammation of synovial membranes, which leads to degradation of articular cartilage and the juxta-articular bone. Inflammation is caused by T cells, B cells, and monocytes when endothelial cells are activated.
Neovascularization, the growth of new blood vessels, serves as an additional marker for rheumatoid arthritis.
A hyperplastic synovial lining layer can be caused by the expansion of synovial fibroblast and macrophage cells.
This expansion of the synovial membrane, sometimes referred to as “pannus”, can lead to bony erosions and cartilage degradation at the site of the cartilage-bone junction in the periarticular bone.
Histologically nodules show a shell of fibrous tissue surrounding a center of fibrinoid necrosis.
Small pea-sized nodules have one center.
Larger rheumatoid nodules tend to be multilocular, with many separate shells or with connections between the necrotic centers.
Individual necrotic centers may open on to a large bursal pocket containing synovial fluid.
The boundary between the necrotic center and the outer fibrous shell is known as a cellular palisade.
The palisade is a densely packed layer of macrophages and fibroblasts which tend to be arranged radially.
In the fibrous shell there is a zone that contains T cells and plasma cells in association with blood vessels.
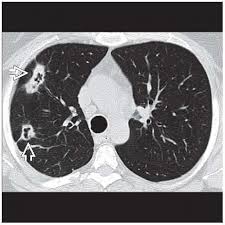
The histology of pulmonary nodules mimics that of subcutaneous nodules, with central necrosis surrounded by palisading macrophages and inflammatory infiltrate.
Risk factors for rheumatoid nodules for people with rheumatoid arthritis may include:
A strong association with smoking
Elevated levels of serum rheumatoid factors
HLA-DRB1 gene with a weak association
Trauma to small vessels
Severe rheumatoid arthritis
Taking Methotrexate over other arthritis drugs
Diagnosis is typically determined clinically.
Rheumatoid arthritis associated rheumatoid nodules are typically subcutaneous and occur at extensor sites.
Rheumatoid nodules onset typically starts in adulthood and presents with rheumatoid factors and bone erosions, and concomitant joint diseases.
Rheumatoid nodulosis is characterized by multiple subcutaneous nodules presenting with rheumatoid factors but an absence of joint complaints.
The nodules are typically small and concentrated on the extensor sites of the hands and feet, sometimes accompanied by bone erosions.
The onset typically starts in adulthood with a pathology similar to rheumatoid arthritis associated rheumatoid nodules.
Such benign rheumatoid nodules are often not associated with rheumatoid factors or concomitant joint diseases.
Benign rheumatoid nodules are typically found on the feet, scalp, and pretibial regions, and are frequently seen in children before the age of 18.
Pathology is similar to that of rheumatoid arthritis associated rheumatoid nodules.
These nodules are non-tender and undergo rapid growth, and also resolve spontaneously.
A similar intracutaneous presentation is known as granuloma annulare.
Rheumatic fever nodules are typically associated with acute rheumatic fever in children.
Rheumatic fever nodules are not accompanied by rheumatoid factors or bone erosions, but are associated with concomitant joint diseases.
No larger than the size of peas, and are typically found at extensor sites and processus spinosi of the vertebrae.
The pathology is characterized by central necrosis and little histiocytic/lymphocytic infiltration.
Four different types of rheumatoid nodules exist: subcutaneous rheumatoid nodules, cardiac nodules, pulmonary nodules and central nervous system nodules.
Subcutaneous rheumatoid nodules:
7% of individuals diagnosed with rheumatoid arthritis reported the presence of subcutaneous rheumatoid nodules upon initial diagnosis.
And about 30–40% of all those diagnosed with rheumatoid arthritis reported developing these nodules throughout the course of the disease.
Subcutaneous rheumatoid nodules is correlated with the increased risk of cardiovascular and respiratory disease.
Cardiac nodules:
Rheumatoid nodules may also form in the heart: myocardium, pericardium, and other valvular structures.
Cardiac nodules are rare.
The reported prevalence of pulmonary nodules has varying depending on the method of detection, from 32% on lung biopsies in rheumatoid arthritis, to 0.4% on plain film radiographs of the chest.
Studies report increased pulmonary nodule growth following treatments with methotrexate, leflunomide, and etanercept.
Nodules developing in the central nervous system is also relatively rare.
Most reports of nodule growth on the central nervous system also presented with severe stages of erosive joint diseases.
Such nodules can be detected through MRI.
There are no methods to completely prevent the development of rheumatoid nodules, but proper management of the disease could reduce the risk of nodule formation.
Additionally, proper medication adherence, smoking cessation, increasing physical activity, could possibly prevent nodules.
Common drug therapies for rheumatoid arthritis may show no benefits towards the treatment for rheumatoid nodules.
Methotrexate, a drug often used in rheumatoid arthritis, is actually correlated with the increased risk of nodule formation.
Rheumatoid nodules may. cause pain or nerve entrapment, and treatment for these symptoms is with nonsteroidal anti-inflammatory drugs.
Corticosteroids, have shown to decrease nodular size, however, it can increase the risk of infection as well.
Local corticosteroid injections seems to be the most common treatment.
Surgery to have the nodule removed is usually indicated in the case of eroding/ necrotising skin.
The lungs are most common in patients with rheumatoid factor who also have subcutaneous nodules.
In the lung can cavitate and lead rarely to bronchopulmonary fistulas.
Cavitating lung nodules may occur in patients with rheumatoid arthritis with occupational exposure to silica, coal dust, or asbestosis and is referred to as Caplan’s syndrome.
