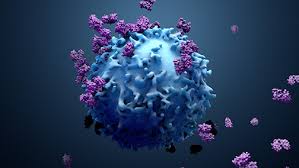
Regulatory T cells (Tregs) are a specialized subset of T cells that play a crucial role in maintaining immune homeostasis and self-tolerance.
Regulatory T cells (Tregs) are primarily characterized by the expression of the transcription factor FOXP3 and the high-affinity interleukin-2 (IL-2) receptor chain CD25.
Tregs are classified into two main types: natural Tregs (nTregs), which develop in the thymus, and induced Tregs (iTregs), which differentiate from conventional T cells in the periphery under specific conditions.
Both types are essential for suppressing excessive immune responses and preventing autoimmune diseases.
Tregs exert their suppressive functions include:
Secretion of inhibitory cytokines such as IL-10 and TGF-β.
Induction of apoptosis in effector T cells.
Cytokine deprivation, leading to apoptosis of effector T cells.
Inhibition of dendritic cell function, thereby reducing antigen presentation and T cell activation.
Treg deficiencies or dysfunctions are associated with various autoimmune and inflammatory diseases, such as Immunodysregulation, Polyendocrinopathy, and Enteropathy, X-linked (IPEX) syndrome.
Conversely, Tregs can also contribute to immune evasion in cancer by suppressing anti-tumor immune responses.
In summaTregs are indispensable for the regulation of immune responses, maintaining self-tolerance, and preventing autoimmune diseases, while also playing a role in the tumor microenvironment.
The regulatory T cells (Treg cells), formerly known as suppressor T cells, are a subpopulation of T cells that modulate the immune system.
Treg cells maintain tolerance to self-antigens, and prevent autoimmune disease.
Regulatory T cells (Tregs) are a specialized subset of CD4+ T cells that play a crucial role in maintaining immune homeostasis and self-tolerance.
They are primarily characterized by the expression of the transcription factor FoxP3, which is essential for their development and function.
Tregs can be broadly categorized into two main types: thymus-derived natural Tregs (nTregs) and peripherally induced Tregs (iTregs).
nTregs develop in the thymus and are identified by the expression of CD25 and FoxP3.
iTregs, on the other hand, are generated from naive CD4+ T cells in the periphery upon antigen exposure and under the influence of specific cytokines such as TGF-β and IL-10.
The primary function of Tregs is to suppress immune responses, thereby preventing autoimmunity and controlling excessive inflammation.
They occurs through several mechanisms, including the secretion of inhibitory cytokines (e.g., IL-10, TGF-β), cytolysis of effector T cells via granzyme-perforin pathways, metabolic disruption of effector T cells, and modulation of dendritic cell function.
Treg dysfunction or deficiency is associated with various autoimmune and inflammatory diseases, such as IPEX syndrome (Immunodysregulation, Polyendocrinopathy, and Enteropathy, X-linked syndrome) and other conditions characterized by uncontrolled immune activation.
Regulatory T cells are essential for maintaining immune tolerance and preventing pathological immune responses, with their function being critically dependent on the transcription factor FoxP3.
Their role in immune regulation makes them a potential target for therapeutic interventions in autoimmune diseases, transplantation, and cancer.
Treg cells are immunosuppressive and generally suppress or downregulate induction and proliferation of effector T cells.
Treg cells express the biomarkers CD4, FOXP3, and CD25.
Treg cells are thought to be derived from the same cell line as naïve CD4+ cells.
Treg cells are very difficult to discern from effector CD4+.
The cytokine transforming growth factor beta (TGF-β) is essential for Treg cells to differentiate from naïve CD4+ cells and is important in maintaining Treg cell homeostasis.
Treg cells in the tumor microenvironment is indicative of a poor prognosis, and Treg cells are thought to suppress tumor immunity, thus hindering the body’s innate ability to control the growth of cancerous cells.
T regulatory cells are a component of the immune system that suppress immune responses of other cells.
It is an important “self-check” built into the immune system to prevent excessive reactions.
Regulatory T cells shut down immune responses after they have successfully eliminated invading organisms, and also in preventing autoimmunity.
CD4+ FOXP3+ CD25 regulatory T cells are naturally occurring regulatory T cells.
All T cells derive from progenitor cells in the bone marrow, which become committed to their lineage in the thymus.
All T cells begin as CD4-CD8-TCR- cells at the double-negative stage, where an individual cell will rearrange its T cell receptor genes to form a unique, functional molecule, which they, in turn, test against cells in the thymic cortex for a minimal level of interaction with self-MHC.
If they receive these signals, they proliferate and express both CD4 and CD8, becoming double-positive cells.
The selection of Tregs occurs on hematopoietically derived MHC class II-expressing cells in the medulla or Hassall’s corpuscles in the thymus.
The process of Treg selection is determined by the affinity of interaction with the self-peptide MHC complex.
A T cell that receives very strong signals will undergo apoptotic death; a cell that receives a weak signal will survive and be selected to become an effector cell.
If a T cell receives an intermediate signal, it will become a regulatory cell.
Tregs highly expressing CD25, GITR (Glucocorticoid-Induced TNFR-Related protein ) and PD-1 are more self-reactive and control lymphoproliferation in peripheral lymph nodes, and may have the ability to protect against autoimmune disorders.
Foxp3+ Treg generation in the thymus is delayed by several days compared to T effector cells and does not reach adult levels in either the thymus or periphery until around three weeks post-partum.
Treg cells require CD28 co-stimulation and B7.2 expression is largely restricted to the medulla, the development of which seems to parallel the development of Foxp3+ cells.
The immune system must be able to discriminate between self and non-self, and when self/non-self discrimination fails, the immune system destroys cells and tissues of the body and as a result causes autoimmune diseases.
Regulatory T cells actively suppress activation of the immune system and prevent pathological self-reactivity, autoimmune disease.
A severe autoimmune syndrome that results from a genetic deficiency in regulatory T cells is the IPEX syndrome.
Regulatory T cells produce a number of inhibitory cytokines: TGF-β, Interleukin and Interleukin 10.
Regulatory T cells can also induce other cell types to express interleukin-10.
Regulatory T cells can produce Granzyme B, which in turn can induce apoptosis of effector cells.
Antigen-activated T cells produce IL-2 which then acts on IL-2 receptors on regulatory T cells alerting them to mount a suppressory response against them to ensure that overreaction is not occurring.
Disruption of this loop leads to hyperreactivity, regulation can modify the strength of the immune response.
A major mechanism of suppression by regulatory T cells is through the prevention of co-stimulation through CD28 on effector T cells by the action of the molecule CTLA-4.
T regulatory lymphocytes develop either in the thymus or in the periphery, and are divided into natural and induced T regulatory cells.
Natural T regulatory lymphocytes (nTregs) are characterized by continuous expression of FoxP3 and T cell receptor (TCR) with relatively high autoaffinity.
Natural T regulatory lymphocyte cells are predominantly found in the body in the bloodstream or lymph nodes and serve mainly to confer tolerance to autoantigens.
Induced peripheral T regulatory cells (iTregs, pTregs) arise under certain situations in the presence of IL-2 and TGF-b in the periphery and begin to express FoxP3 inducibly, thus becoming the functional equivalent of tTreg cells.
iTregs,are found primarily in peripheral barrier tissues, involved in preventing inflammation in the presence of external antigens.
The main differentiating features of tTreg and iTreg cells include Helios and Neuropilin-1, the presence of which suggests origin in the thymus.
And the two Treg cell populations differ in is the stability of FoxP3 expression in different settings.
Induced regulatory T (iTreg) cells (CD4+ CD25+ FOXP3+) are suppressive cells involved in tolerance, suppressing
T cell proliferation and experimental autoimmune diseases.
These cells include Treg17 cells.
iTreg cells develop from mature CD4+ conventional T cells outside of the thymus: a defining distinction between natural regulatory T (nTreg) cells and iTreg cells.
Epigenetic differences between nTreg and iTreg cells, with the former having more stable FOXP3 expression and wider demethylation.
The small intestinal environment is high in vitamin A and is a location where retinoic acid is produced.
The retinoic acid and TGF-beta produced by dendritic cells within this area signal for production of regulatory T cells.
Regulatory T cells cells are associated with the functions of mucosal lymphoid tissues such as the intestinal barrier.
In the intestinal lamina propria, 20-30% of Foxp3+ T regulatory cells are found and this high proportion is strongly dependent on the presence of a complex gut microbiome.
Induction of RORγt+ Treg cells in lymph nodes of the small intestine is crucial for the establishment of intestinal luminal antigen tolerance,and these cells are particularly important in the prevention of food allergies.
These cells inhibit the production of suppressive molecules such as the cytokine IL-10, and also suppress the Th17 cell population and inhibit the production of IL-17, thus suppressing the pro-inflammatory response.
A subset of Treg cells are Gata3+ Treg cells, which respond to IL-33 in the gut and influence the regulation of effector T cells during inflammation.
Gata3+ T regs are major immunosuppressors during intestinal inflammation and T regs use Gata3 to limit tissue inflammation.
Immunosuppressive function of regulatory T cells prevents the development of autoimmune disease, it is not desirable during immune responses to infectious microorganisms.
Upon encounter with infectious microorganisms, the activity of regulatory T cells may be downregulated, either directly or indirectly, by other cells to facilitate elimination of the infection.
Some pathogens can manipulate regulatory T cells to immunosuppress the host and so potentiate their own survival:
Regulatory T cell activity has been reported to increase in several infectious diseases: retroviral infections, mycobacterial infections and various parasitic infections including Leishmania and malaria.
Treg cells play a significant role during HIV infection, as they suppress the immune system, thus limiting target cells and reducing inflammation, but this simultaneously disrupts the clearance of virus by the cell-mediated immune response and enhances the reservoir by pushing CD4+ T cells to a resting state, including infected cells.
Treg cells can be infected by HIV, increasing the size of the HIV reservoir directly.
Regulatory T cells have a large role in the pathology of leishmaniasis.
Increased numbers of regulatory T cells in breast, colorectal and ovarian cancers are associated with a poorer prognosis.
There is some evidence that Treg cells may be dysfunctional and driving neuroinflammation in amyotrophic lateral sclerosis due to lower expression of FOXP3.
Regulatory T cells increase via polyclonal expansion both systemically and locally during healthy pregnancies to protect the fetus from the maternal immune responsea process called maternal immune tolerance.
Polyclonal expansion may be impaired in preeclamptic mothers and their offspring.
Most cancers elicit an immune response in the host that is mediated by tumor antigens, thus distinguishing the tumor from other non-cancerous cells.
There are large numbers of tumor-infiltrating lymphocytes (TILs) to be found in the tumor microenvironment.
Treg cells seem to be preferentially trafficked to the tumor microenvironment.
Treg cells normally make up only about 4% of CD4+ T cells, they can make up as much as 20–30% of the total CD4+ population around a tumor microenvironment.
The ratio of Treg to effector T cells in the tumor microenvironment is a determining factor in the success of the immune response against the cancer.
High levels of Treg cells in the tumor microenvironment are associated with poor prognosis in many cancers: ovarian, breast, renal, and pancreatic cancer.
Treg cells suppress effector T cells and hinder the body’s immune response against the cancer.
In some types of cancer the opposite is true, and high levels of Treg cells are associated with an improved prognosis: colorectal carcinoma and follicular lymphoma.
Treg cells’ role in the development of cancer is highly dependent on both type and location of the tumor.
Treg infiltration into the tumor microenvironment is facilitated by the binding of the chemokine receptor CCR4, which is expressed on Treg cells, to its ligand CCL22, which is secreted by many types of tumor cells.
The cytokine, TGF-β, commonly produced by tumor cells, is known to induce the differentiation and expansion of Treg cells.
Forkhead box protein 3 (FOXP3) as a transcription factor is an essential molecular marker of Treg cells.
FOXP3 polymorphism might be involved in the gastric cancer progression through influencing Treg function and the secretion of immunomodulatory cytokines such as IL-10, IL-35, and TGF-β.
The immunosuppression of the tumor microenvironment has largely contributed to the unsuccessful outcomes of many cancer immunotherapy treatments.
Depletion of Treg cells in animal models has shown an increased efficacy of immunotherapy treatments,
Anti-CTLA-4 antibodies cause depletion of Tregs and thus increase CD8+ T cells effective against tumors.
Anti-CTLA-4 antibody ipilimumab was approved for patients with advanced melanoma.
Immune-checkpoint molecule PD-1 inhibits activation of both conventional T cells and Tregs and use of anti-PD-1 antibodies may lead to activation and immunosuppressive function of Tregs.
Resistance to anti-PD-1-mAb treatment is probably caused by enhanced Treg cell activity.
Rapid cancer progression upon PD-1 blockade is called hyperprogressive disease.
Therapy targeting TCR signaling by blocking tyrosine kinases, as is used for treatment of chronic myeloid leukemia and is associated with Treg inhibition.
Regulatory T cells are defined by expression of the forkhead family transcription factor FOXP3.
Expression of FOXP3 is required for regulatory T cell development and appears to control a genetic program specifying this cell’s fate.
The large majority of Foxp3-expressing regulatory T cells are found within the major histocompatibility complex (MHC) class II restricted CD4-expressing (CD4+) population and express high levels of the interleukin-2 receptor alpha chain (CD25).
These FOXP3-expressing CD8+ T cellls appear to be induced in autoimmune disease states by T cell receptor stimulation to suppress IL-17-mediated immune responses.
Unlike conventional T cells, regulatory T cells do not produce IL-2 and are therefore anergic at baseline.
Regulatory T cells comprise about 5–10% of the mature CD4+ T cell subpopulation while about 1–2% of Treg can be measured in whole blood.
Regulatory T cells play a critical role in maintaining normal immune system function: mutations in FOXP3 develop a severe and rapidly fatal autoimmune disorder known as Immune dysregulation, Polyendocrinopathy, Enteropathy X-linked (IPEX) syndrome.
The IPEX syndrome is characterized by the development of overwhelming systemic autoimmunity in the first year of life.
With IPEX there is commonly observed triad of watery diarrhea, eczematous dermatitis, and endocrinopathy seen most commonly as insulin-dependent diabetes mellitus.
Most individuals have other autoimmune phenomena including Coombs-positive hemolytic anemia, autoimmune thrombocytopenia, autoimmune neutropenia, and tubular nephropathy.
The majority of affected males die within the first year of life of either metabolic derangements or sepsis.
