 The recurrent laryngeal nerve (RLN) is a branch of the vagus nerve (cranial nerve X) that supplies all the intrinsic muscles of the larynx, with the exception of the cricothyroid muscles.
The recurrent laryngeal nerve (RLN) is a branch of the vagus nerve (cranial nerve X) that supplies all the intrinsic muscles of the larynx, with the exception of the cricothyroid muscles.
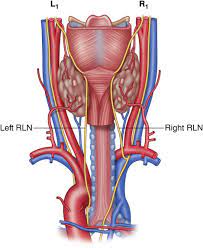
There are two recurrent laryngeal nerves, right and left.
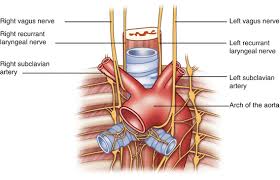
Right recurrent laryngeal nerve branches from the vagus nerve at the level of the subclavian artery, travels behind this artery and ascends to the neck.
The right and left nerves are not symmetrical, with the left nerve looping under the aortic arch, and the right nerve looping under the right subclavian artery then traveling upwards.
The right recurrent laryngeal nerve travels in the tracheo-esophageal groove and is lateral in the lower neck and medial in the upper neck.
They both travel alongside the trachea.
The nerves are among the few nerves that follow a recurrent course, moving in the opposite direction to the nerve they branch from, a fact from which they gain their name.
In about 0.5% of patients the right recurrent laryngeal nerve is not recurrent and directly goes from the vagus nerve at the level of the cricothyroid cartilage and enters the cricothyroid muscle.
On the left side the nerve branches from the vagus nerve and passes below the aortic arch, then reverses its course superiorly and posterior associated it enters the neck.
On the left the nerve travels within the tracheo-esophageal groove and enters below the aorta.
The right RLN loops around the right subclavian artery.
The left RLN has a longer intrathoracic course than the right RLN and is therefore more likely to suffer injury.
Injury to the RLN may result in vocal cord paralysis.
Unilateral vocal cord paralysis can cause dysphonia, low pitched voice, vocal fatigue, dysphagia, and choking.
With bilateral vocal paralysis, phonation can be nearly normal.
Recurrent laryngeal nerve palsy may be caused by intra-thoracic or extra thoracic processes.
The recurrent laryngeal nerves supply sensation to the larynx below the vocal cords, give cardiac branches to the deep cardiac plexus, and branch to the trachea, esophagus and the inferior constrictor muscles.
The posterior cricoarytenoid muscles, the only muscles that can open the vocal folds, are innervated by this nerve.
The recurrent laryngeal nerves are the nerves of the sixth pharyngeal arch.
Passing under the subclavian artery, the right recurrent laryngeal nerve has a much shorter course than the left which passes under the aortic arch and ligamentum arteriosum.
The recurrent laryngeal nerves branch from the vagus nerve, relative to which they get their names; indicates they run in the opposite direction to the vagus nerves from which they branch.
The vagus nerves run down into the thorax, and the recurrent laryngeal nerves run up to the larynx.
The vagus nerves, from which the recurrent laryngeal nerves branch, exit the skull at the jugular foramen and travel within the carotid sheath alongside the carotid arteries through the neck.
The recurrent laryngeal nerves branch off the vagus, the left at the aortic arch, and the right at the right subclavian artery.
The left RLN passes in front of the arch, and then wraps underneath and behind it.
The nerves typically ascend in a groove at the trachea and esophagus, and then pass behind the posterior, middle part of the outer lobes of the thyroid gland and enter the larynx underneath the inferior constrictor muscle, passing into the larynx just posterior to the cricothyroid joint.
The terminal branch is the inferior laryngeal nerve.
The right and left RLNs lack bilateral symmetry.
The left RLN is longer than the right, as it crosses under the arch of the aorta at the ligamentum arteriosum.
Somatic motor fibers that innervate the laryngeal muscles, and pharyngeal muscles are located in the nucleus ambiguus and emerge from the medulla in the cranial root of the accessory nerve.
Fibers cross over to and join the vagus nerve in the jugular foramen.
Sensory cell bodies are located in the inferior jugular ganglion, and the fibers terminate in the solitary nucleus.
Parasympathetic fibers to segments of the trachea and esophagus in the neck originate in the dorsal nucleus of the vagus nerve.
In about 1 of 100–200 people, the right inferior laryngeal nerve is nonrecurrent, in that branches off the vagus nerve around the level of the cricoid cartilage.
Such a configuration is accompanied by variation in the arrangement of the major arteries in the chest; most commonly, the right subclavian artery arises from the left side of the aorta and crosses behind the esophagus.
A left nonrecurrent inferior laryngeal nerve is even more uncommon, as it requires the aortic arch be on the right side, accompanied by an arterial variant which prevents the nerve from being drawn into the chest by the left subclavian.
In about four of five individuals, there is a connecting branch between the inferior laryngeal nerve, a branch of the RLN, and the internal laryngeal nerve, a branch of the superior laryngeal nerve (anastomosis of Galen).
As the recurrent nerve hooks around the subclavian artery or aorta, it gives off several branches to the cardiac plexus, trachea, esophagus and inferior pharyngeal constrictor muscle.
The recurrent laryngeal nerves control all intrinsic muscles of the larynx except for the cricothyroid muscle.
The intrinsic muscles of the larynx act to open, close, and adjust the tension of the vocal cords, and include the posterior cricoarytenoid muscles, the only muscle to open the vocal cords.
The nerves supply muscles on the same side of the body, with the exception of the interarytenoid muscle, which is innervated from both sides.
Branches of the recurrent laryngeal nerve also carry sensory information from the mucous membranes of the larynx below the lower surface of the vocal fold, and sensory, secretory and motor fibres to the cervical segments of the esophagus and the trachea.
The recurrent laryngeal nerves may be injured as a result of trauma, during surgery, or as a result of tumor spread.
Injury to the recurrent laryngeal nerves can result in hoarseness or loss of voice and cause problems in the respiratory tract.
Injury to the nerve may paralyze the posterior cricoarytenoid muscle on the same side.
The posterior cricoarytenoid muscle is the sole muscle responsible for opening the vocal cords, and paralysis may cause dyspnea during physical activity.
Injury to both the right and left nerve may result in more serious damage, such as the inability to speak.
During healing nerve fibers that re-anastamose may result in vocal cord motion impairment, uncoordinated movements of the vocal cord.
The RLN is at risk for injury during neck surgery, especially thyroid and parathyroid surgery; as well as esophagectomy.
RLN nerve damage can be assessed by laryngoscopy, during which a to confirm the absence of movement in the affected side of the vocal cords.
The right recurrent laryngeal nerve is more susceptible to damage during thyroid surgery because it is close to the bifurcation of the right inferior thyroid artery.
Thermal injury to the RLN can occur with the use of radio frequency ablation to remove thyroid nodules.
The RLN is permanently damaged in 0.3–3% of thyroid surgeries, and transient paralysis occurs in 3–8% of surgeries.
Recurrent laryngeal nerve damage is one of the leading causes of medicolegal issues for surgeons.
No difference between visually identifying the RL nerve or utilizing intraoperative neuroimaging during surgery, to prevent injury to the nerve during surgery.
2–18% of lung cancer patients develop hoarseness because of recurrent laryngeal nerve compression, usually left-sided: it often indicates inoperable tumors.
Thyroid surgery, cervical spine surgery, carotid artery surgery, skull-base operations account for most common causes of damage to the recurrent laryngeal nerve.
Thyroid goiters or malignant lesions such as lymphomas, skull tumors, neurologic disorders, toxins, radiation, chemotherapy agents, viral infections and endotracheal intubation may damage this nerve.
15% of cases are associated with idiopathic recurrent laryngeal nerve palsy.
