 Pulsed field ablation (PFA) is a non-thermal, not using extreme heat or cold, method of biological ablation utilizing high-amplitude pulsed (microsecond duration) electric fields to create irreversible electroporation in tissues.
Pulsed field ablation (PFA) is a non-thermal, not using extreme heat or cold, method of biological ablation utilizing high-amplitude pulsed (microsecond duration) electric fields to create irreversible electroporation in tissues.
It is used most widely to treat cancer or cardiac arrhythmias.
Atrial fibrillation frequently results from bursts of tachycardia that originate in muscle bundles extending from the atrium to the pulmonary veins.
Pulmonary vein isolation ablation technology has used thermal methods (radiofrequency ablation or, less often, cryoablation) to destroy pulmonary vein cells.
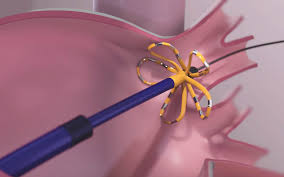
In pulsed field ablation, a thin, flexible catheter is inserted into a blood vessel in the groin and threaded up into the heart to ablate the areas of the pulmonary vein causing excessively rapid electrical signals.
In one study, atrial fibrillation recurrence in the thermal ablation group was 39% compared to 11% in the PFA group.
PFA can achieve pulmonary vein isolation faster than other ablation methods.
Compared to radiofrequency ablation, PFA produces lesions of greater uniformity.
Cell death following PFA is usually due to apoptosis.
Apoptosis is a far less damaging and inflammatory form of cell death than necrosis.
In contrast to thermal methods of ablation, PFA specifically kill without injuring surrounding tissues.
Thermal ablation methods can damage the esophagus, phrenic nerve, and coronary vessels (as high as 5% ) which are spared by PFA.
The complication rate PFA is 0.7% with no occurrence of phrenic nerve, esophageal, or pulmonary vein injury.
Recent comparisons of PFA with thermal methods have shown reduced time spent in surgery, but no superiority in safety and no better reduction of atrial fibrillation.
