 Sarcoidosis predominant involves lungs and intrathoracic lymph nodes.
Sarcoidosis predominant involves lungs and intrathoracic lymph nodes.
Chest x-rays are abnormal in 80% to more than 90% of patients with sarcoidosis.
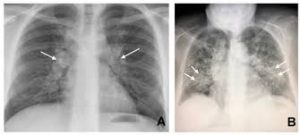
Classic chest x-ray findings of sarcoidosis is bilateral hilar lymphadenopathy, which occurs in at least 40% of patients, often with prominent right paratracheal lymphadenopathy.
Enlarged mediastinal, subcarinal, or hilar nodes are present in approximately 80% of patients with sarcoidosis.
Pulmonary parenchymal infiltrates alone are present in 16% of patients with sarcoidosis and occur with lymphadenopathy in more than 40% of patients.
Parenchymal infiltrates are usually bilateral and predominantly central in the upper lobes of the lung.
Chronic fibrosis causing pulmonary volume loss, hilar retraction, architectural distortion, bronchiectasis, bullae, and cystic radiolucencies may be seen.
Black individuals typically present with more advanced x-ray disease compared with white individuals, stage for stage in pulmonary sarcoidosis.
Physicalexamination of the chest is often unremarkable.
Pulmonary function tests are normal in more than 80% of patients without parenchymal infiltrates on chest x-rays.
The Scadding staging system by chest x-ray for pulmonary sarcoidosis includes five stages: zero is normal, I bilateral hilar adenopathy without pulmonary infiltrates, II bilateral hilar lymphadenopathy with pulmonary infiltrates, III pulmonary infiltrates without bilateral hilar lymphadenopathy and IV extensive fibrosis and distortion or bullae.
Fiber-optic bronchoscopy with transbronchial lung biopsy is sensitive to diagnose pulmonary sarcoidosis in 60 to 90% of cases when pulmonary infiltrates are present on chest x-ray.
A cobblestone appearance in airways in the airways often reflect
bronchial involvement.
Endobronchial biopsies of abnormal appearing airways should be performed.
If mediastinal lymph nodes are enlarged, an endobronchial ultrasound trans bronchial needle aspiration has a sensitivity of 80% or greater.
The differential diagnosis in patients with cough, dyspnea and x-rays suggesting sarcoidosis include:
tuberculosis and other granulomatous infections, fungi, lymphoma, granulomatous and lymphocytic interstitial lung disease, rheumatoid nodules, Langerhans cell histiocytosis, IgG 4 related disease, inflammatory bowel disease and primary biliary cirrhosis, hypersensitivity pneumonitis, pneumoconiosis, drug induced granulomatous disease such as interferon, checkpoint inhibitors, antitumor necrosis factor, berylliosis, and foreign body granulomatosis.
High resolution CT chest scans are superior to chest radiographs in assessing sarcoidosis lung involvement.
CT of the chest imaging increases the likelihood of diagnosing active lung inflammation and can quantify lung fibrosis, which may alter treatment and prognosis.
Typical findings on high resolution CT of the chest in pulmonary sarcoidosis includes micronodules, in a perilymphatic and central distribution, consolidation, parahilar opacities, and fibrosis.
Less commonly CT scans may show mass like or alveolar opacities, ground glass opacities, military opacities and cavitation.
In long-standing sarcoidosis calcified nodes occur in more than 50% of patients.
Prognosis: patients who present with erythema nodosum, Lofgren syndrome, stage I disease, improvement in disease or resolution of disease have a favorable prognosis.
Studies suggest that radiographic resolution of 49 to 82% for stage I, 31 to 68% for stage II, 10% to 38% for stage III, and 0% for stage IV in patients followed between one and 15 years.
Approximately 75 to 85% of spontaneous remission’s occur within two years of presentation.
White patients followed for mean of nine years have sustained remission rates of 50% while BTlack individuals are 20%.
Patients with more extensive lung involvement, extra pulmonary organ involvement such as chronic cutaneous sarcoidosis, bone involvement or multiorgan involvement, lower income, Black race, and need for treatment are associated with poor prognosis.
Mortality rates due to sarcoidosis are higher than the general population.
Black individuals have higher mortality rates (females 10 per 1,000,000, males, 3 deaths per 1 million and whites 1 per million individuals.
Precapillary pulmonary hypertension, may occur in patients with sarcoidosis, especially if there is fibrotic and cystic lung disease involvement.
Precapillary pulmonary hypertension is associated with a poor prognosis and a five-year survival rate of 59% compared with 95% for those patients with sarcoidosis without precapillary pulmonary hypertension.
TREATMENT:
Oral glucocorticoids are the primary therapy for pulmonary sarcoidosis.
Azothioprine and methotrexate are secondary line therapies for pulmonary sarcoidosis, and are prescribed for patients unable to reduce the prednisone dose to less than 10 mg a day.
Third line therapies include mycophenolate mofetil and antitumor necrosis factor agents.
