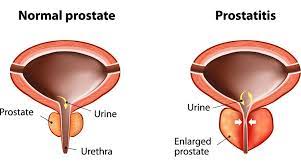
 Prostatitis is a common condition of series of disorders, ranging from acute bacterial infection to chronic pain syndromes, in which the prostate gland is inflamed.
Prostatitis is a common condition of series of disorders, ranging from acute bacterial infection to chronic pain syndromes, in which the prostate gland is inflamed.
About a 5-9 percent lifetime prevalence.
About 15 percent of men who see a physician for genitourinary complaints are diagnosed with prostatitis.
Approximately 2 million physician visits include the diagnosis of prostatitis, annually.
Prostatitis is not easily diagnosed.
Patients often present with varied, nonspecific symptoms, and the physical examination is frequently not helpful.
Prostatitis symptoms include: urinary obstruction, fever, myalgias, decreased libido or impotence, painful ejaculation and low-back and perineal pain.
Divided into acute and chronic bacterial prostatitis and chronic abacterial prostatitis and granulomatous prostatitis.
Refers to wide array of symptoms from infection of the prostate to chronic pelvic pain without infection, and histologic evidence of prostatic inflammation without symptoms.
Accounts for an estimated 2 million visits to physicians per year in the U.S.
Acute prostatitis usually characterized by dysuria and fever with acute infection of E .Coli, Klebsiella, Enterobacter and Pseudomonas.
Physical examination often fails to clarify the cause of the pain.
Because occult prostatectomy infection often exists cultures and microscopic examination of urine and prostatic secretions before and after prostatic massage may help differentiate prostatitis caused by infection from prostatitis with other causes.
Because occult prostatectomy infection often exists, a therapeutic trial of antibiotics is often in order even when patients do not appear to have bacterial prostatitis.
Antibiotics are continued for at least three to four weeks.
Acute prostatitis associated with urinary frequency, urgency, hesitancy and burning on urination.
Less commonly Staphylococcus aureus, Streptococcus faecalis, Chlamydia or anaerobes such as Bacteriodes species are involved in acute bacterial prostatitis.
ABP patients may have findings consistent with cystitis or pyelonephritis, as well .
Patients with ABP may present with fever, chills, low back pain, perineal or ejaculatory pain, dysuria, urinary frequency, urgency, myalgias and varying degrees of obstruction.
The prostate gland on examination is tender, warm, swollen, firm and irregular.
Avoiding vigorous digital examination of the infected prostate is appropriate because it that may induce or worsen bacteremia.
In acute bacterial prostatitis, the infecting organism can often be identified by culturing the urine.
Antibiotic selection is initially empiric, to be modified once pathogen susceptibilities are available.
Many antibiotics cross the blood-prostate barrier poorly, and efficacy of antibiotic treatment is probably limited.
The inability of many antibiotics to penetrate the prostatic epithelium when it is not inflamed, causes limited antibiotic efficacy.
More lipophilic antibiotics can better cross the prostate lipid membrane epithelial barrier.
Commonly used agents include:
tetracycline, trimethoprim-sulfamethoxazole, or a quinolone.
Other medications indicated for treatment of prostatitis include: carbenicillin, cefazolin, cephalexin, cephradine and
The duration of therapy is recommended to be continued for three to four weeks to prevent relapse.
Most practiotiomers use TMP-SMX as the first-line agent in treating prostatitis.
TMP-SMX is considered a first-line antibiotic for chronic bacterial prostatitis caused by gram-negative bacteria.
In severely ill patients hospitalization for parenteral antibiotics, usually a broad-spectrum cephalosporin and an aminoglycoside.
Massaging or repeat prostate examinations in the presence of acute prostatitis can lead or bacteria and urosepsis.
Acute prostatitis evaluation should include measuring of postvoid residual urine preferably by ultrasound to avoid urinary cauterization, urinalysis, urine and blood cultures.
Four types of prostatitis, Chronic prostatitis/chronic pelvic pain syndrome, chronic bacterial prostatitis, acute (sudden) bacterial prostatitis, and asymptomatic inflammatory prostatitis.
Prostatitis is divided into four subtypes based on the chronicity of symptoms, the presence of white blood cells in the prostatic fluid and culture results.
These subtypes are:
acute bacterial prostatitis,
chronic bacterial prostatitis,
chronic nonbacterial prostatitis
prostadynia.
Chronic prostatitis/chronic pelvic pain is the most common form.
Chronic nonbacterial prostatitis and prostadynia are merged into a category called chronic nonbacterial prostatitis/chronic pelvic pain syndrome.
Acute bacterial prostatitis (ABP) is considered a subtype of urinary tract infection.
ABP is due to reflux of infected urine into the prostate via the ejaculatory and prostatic ducts, or from ascending urethral infection from the meatus, particularly during sexual intercourse.
ABP causative agents are primarily gram-negative, coliform bacteria:
The most commonly found organism is Escherichia coli.
Other bacteria frequently found include in ABP are Klebsiella, Proteus, Enterococci and Pseudomonas.
Less commonly Staphylococcus aureus, Streptococcus faecalis, Chlamydia or anaerobes such as Bacteriodes species are involved in acute bacterial prostatitis.
Chronic prostatitis associated with genitourinary pain with or without voiding symptoms in the absence of urologic bacteria.
Patients with chronic bacterial prostatitis typically have recurrent urinary tract infections with persistence of the same strain of pathogenic bacteria in prostatic fluid or urine.
Chronic bacterial prostatitis symptoms are often variable:irritative voiding symptoms, possibly with pain in the back, testes, epididymis or penis, with low-grade fever, arthralgias and myalgias.
Patients are often asymptomatic between episodes of acute cystitis.
The cure rate for chronic bacterial prostatitis ranges from 33 to 71 percent.
Some men require long-term antibiotic suppression to prevent recurrent urinary tract infections.
Rarely, transurethral prostatectomy can be curative if all of the infected prostatic tissue is removed; however, infection often is harbored in the more peripheral tissues.
The Stamey-Meares four-glass localization method differentiates then types of prostatitis.
Bacterial cultures of the initial voided urine (VB1), midstream urine (VB2), expressed prostatic secretions (EPS), and a postprostatic massage urine specimen (VB3).
The VB1 is a testfor urethral infection or inflammation.
The VB2 is a test for urinary bladder infection.
The prostatic secretions are cultured and analyzed for increased white blood cells, with more than 10 to 20 per high-power field is considered abnormal.
A postmassage urine specimen is believed to flush out bacteria from the prostate that remain in the urethra.
These tests are cumbersome and expensive, and infrequently used.
An alternative diagnostic test, the pre- and postmassage test (PPMT) is easier to carry out, and performs about as well as the four-glass method.
Chronic bacterial prostatic is presents with negative pre-massage urine culture results, and greater than 10 to 20 white blood cells per high-power field in both the pre- and the postmassage urine specimen.
The presence of bacteriuria in the postmassage urine specimen suggests chronic bacterial prostatitis.
Treatment of Prostatitis
Supportive measures for prostatic include antipyretics, analgesics, hydration and stool softeners.
Some patients require antibiotic treatment for several months
If a patient does not respond to antibiotics they may have chronic nonbacterial prostatitis.
Chronic nonbacterial prostatitis:
nonsteroidal anti-inflammatory drugs, alpha-blocking agents, anticholinergic agents may be helpful.
Chronic prostatitis may be a neurogenic pain syndrome.
The chronic non bacterial prostatitis and chronic pelvic pain syndrome symptoms: painful ejaculation or pain in the penis, testicles or scrotum, low back pain, rectal or perineal pain, or even pain along the inner aspects of the thighs.
Additionally, patients with chronic non bacterial prostatitis and chronic pelvic pain syndrome often have obstructive urinary symptoms and decreased libido or impotence.
Patients with chronic non bacterial prostatitis and chronic pelvic pain syndrome can be differentiated from other types of prostatitis by using the Stamey-Meares localization method: sterile cultures, with increased WBCs in prostatic secretions.
The treatment of non bacterial prostatitis and chronic pelvic pain syndrome condition is associated with limited evidence to support any particular therapy: because of a ihigh rate of occult infection an antibiotic trial is reasonable.
Coverage should include
Chlamydia trachomatis, Ureaplasma urealyticum and Mycoplasma hominis.
Options include doxycycline (Vibramycin) or minocycline (Minocin).
In extreme cases, total prostatectomy may provide a cure.
Chronic non bacterial prostatitis and chronic pelvic pain syndrome etiology is not known.
Some cases represent chronic bacterial prostatitis not diagnosed.
Some cases of chronic bacterial prostatitis have increased prostatic uric acid, bladder outflow or pelvic floor muscle disorders, resemble interstitial cystitis or fibromyalgia, without verification.
With long standing chronic prostatitis/chronic pelvic pain syndrome a history of other neurological disease is almost 5 times more likely than in controls (Pontari MA et al).
Possible treatments include: allopurinol, prostate massage, transurethral microwave thermotherapy, Diazepam,
biofeedback, relaxation techniques, muscle relaxants, sitz baths and nonsteroidal anti-inflammatory drugs (NSAIDs).
In individuals enhanced symptoms with alcohol or spicy foods may occur and should be avoided.
Irritative voiding symptoms may be abated with anticholinergic agents, such as oxybutynin, or alpha-blocking agents such as doxazosin, prazosin,tamsulosin [Flomax] or terazosin [Hytrin]).
Reassurance is useful in chronic pain syndromes.
Rarely suprapubic catheters are placed in patients who have severe obstructive symptoms from an acutely inflamed prostate gland.
A prostatic abscess is considered to be present with a prolonged course that does not respond to appropriate antibiotic therapy.
A prostatic abscess can identified as a fluctuant mass on rectal examination, with CT, magnetic resonance imaging or transrectal ultrasonography providing image verification.
A drainage procedure or resection of the abscess is usually required.
Symptomatic and asymptomatic bacterial prostatitis can elevate the PSA test to abnormal levels.
The PSA level returns to normal four to six weeks after a 14-day course of antibiotics for prostatitis.
Treatment is recommended only in patients with chronic asymptomatic prostatitis known to elevate the PSA level.
