Preventing cardiovascular disease (CVD) involves a comprehensive approach that addresses multiple lifestyle and medical factors.
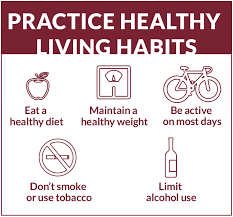
1. Lifestyle Modifications – Maintain a heart-healthy diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats – Engage in regular physical activity (at least 150 minutes of moderate-intensity exercise per week) – Maintain a healthy body weight – Quit smoking and avoid exposure to secondhand smoke – Limit alcohol consumption
2. Medical Management – Regular health screenings to monitor: * Blood pressure * Cholesterol levels * Blood glucose – Manage underlying conditions like diabetes, hypertension, and high cholesterol with medications
3. Diet Recommendations – Reduce saturated and trans fat intake – Increase consumption of omega-3 fatty acids – Limit sodium intake – Eat more fiber-rich foods – Control portion sizes
4. Stress Management – Practice stress-reduction techniques like meditation, yoga, or deep breathing – Ensure adequate sleep (7-9 hours per night) – Maintain healthy social connections – Consider counseling or therapy if experiencing chronic stress
5. Risk Factor Reduction – Control blood pressure (aim for below 120/80 mmHg) – Manage cholesterol levels – Maintain healthy blood sugar levels – Reduce inflammatory markers through diet and lifestyle
6. Advanced Prevention Strategies – Consider aspirin therapy for high-risk individuals (under medical supervision) – Regular cardiovascular risk assessments – Genetic screening for hereditary heart disease risks
By implementing these strategies, individuals can significantly reduce their risk of developing cardiovascular disease and improve overall heart health.
A single combined measure of high sensitivity, CRP, LEL cholesterol, and lipoprotein (a) levels among initially healthy US women was predictive of incident cardiovascular events during a 30 year period: data supports efforts to extend strategies for the primary prevention of atherosclerotic events, beyond traditional, 10 year estimates of risk(Riker PM).
Lipoprotein (a) levels are determined genetically and are stable overtime, and measurement is recommended once without the need for repeat evaluation.
Prevention guidelines, addressing diet, exercise, smoking sensation, and stress reduction consistently show greater benefit when behavioral interventions are implemented earlier in life.
Behavioral modifications can reduce high sensitivity CRP and LDL cholesterol levels, but they do not typically reduce lipoprotein (a) levels, which are largely determined genetically.
Inhibiting inflammation in addition to lowering lipid levels, reduces cardiovascular risk, and one anti-inflammatory agent at low dose, colchicine 0.5 mg daily, has been approved for secondary prevention of atherosclerotic disease and for primary prevention in high risk patients.
Pharmacologic intervention medications to reduce LDL cholesterol clearly lowers cardiovascular risk and is the most important pharmacological tool for risk reduction beyond lifestyle change.
