
 Postmenopausal osteoporosis (PO) is caused by estrogen deficiency.
Postmenopausal osteoporosis (PO) is caused by estrogen deficiency.
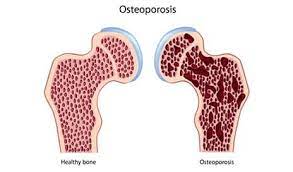
This leads to increased osteoclast differentiation and activation, accelerating bone reabsorption that outpaces formation, and rapid bone loss, particularly in the years immediately before, and after menopause.
PO results in low bone mineral density, deterioration of bone micro architecture, impaired bone strength, and increase in the risk of fragility fractures.
Decreases in bone mineral density is almost universal among postmenopausal women and starts before menopause with an average loss of bone density of 0.5 to 1% per year thereafter.
The diagnosis of PO is established by the occurrence of a fragility fracture without associated trauma or a minor fall, bone mineral density at the spine, hip or femoral neck that is at least 2.5 standard deviations below the mean of the young adult reference population as measured by the use of Dual x-ray absorptiometry (DXA).
In the USA, approximately 20% of women over 50 years of age and 30% of women 65 years of age or older have criteria for osteoporosis.
At menopause, women have a lifetime risk of fracture of more than 50%.
Osteoporosis is more common among White, Asian, and Hispanic, females than Black women.
Approximately 40% of postmenopausal women have low bone mass of osteopenia with T score between minus 1and -2.49.
Approximately 50% of postmenopausal women will have a fragility fracture.
After a hip fracture, many women never regain independence, 20% are institutionalized, and the risk of death within one year doubles.
Black women who have hip fractures
are more likely to die within six months, less likely to gain independence and have timely surgery and rehab and white women who have hip fractures.
The annual healthcare cost with fractures related to postmenopausal osteoporosis is currently $57 billion in the US.
Osteoporosis is asymptomatic until the first clinical fracture.
DXA is the gold standard for identifying patients at risk.
Each standard deviation reduction below a score of zero on the T score is associated with the doubling or tripping in the risk of fracture.
Most guidelines, recommend DEXA of spine and hip for postmenopausal women, 65 years of age or older, and for postmenopausal women younger than 65 who have high risk factors.
Fragility fractures of the spine, hip, forearm, humerus, and pelvis are diagnostic of osteoporosis, even when T score is higher than, -2.5.
Approximately half the women who have reached menopause have fragility fractures.
Approximately 75% of fragility fractures among women who have menopause occur in those with bone mineral density that is normal or that is indicative of osteopenia, with the remaining 25% of fractures occurring in the small population of women with bone mineral density indicative of osteoporosis (T score of less than -2.5).
Fragility fractures are associated with a marked increase in the eminent risk of additional fractures.
The most common osteoporotic fractures, are vertebral compression fractures, which are frequently painful, cause heightloss, but may be asymptomatic.
A vertebral fracture analysis or spine radiography can be performed when osteoporosis suspicion is high or treatment management is affected.
Vertebral fracture analysis has low radiation spine imaging on a densitometer with a high sensitivity and specificity to detect, moderate or severe vertebral compressions.
Vertebral fracture is associated with increased mortality.
Bone microarchitecture contributes to bone strength and can be assessed by a trabecular bone score, an indirect measure of spine trabecular microarchitecture obtained from a DXA imaging with use of additional software any can predict fracture risk independent of bone mineral density.
Evaluation of postmenopausal osteoporosis includes ruling out osteomalacia and other conditions associated with osteoporosis, including the use of glucocorticoids.
TREATMENT:
Goals of treatment, are to prevent fractures in women at higher risk, or to prevent subsequent fractures – primary and secondary prevention.
Lifestyle changes are encouraged, including stoppage of smoking, avoiding excessive alcohol, increased weight-bearing exercise and fall prevention.
Most guidelines recommend 1000 to 1200 mg of calcium daily, preferably obtained from diet and 400 to 1000 international units of vitamin D daily.
Adjusting vitamin D intake to achieve serum 25 hydroxyvitamin D levels higher than 20 to 30 mg nanograms per milliliter is suggested by some.
Calcium and vitamin D supplementation fracture reduction is debated.
Supplementation with calcium and vitamin D significantly reduces hip fracture, but not vertebral or non-vertebral fractures in postmenopausal osteoporosis.
Risk associated with calcium supplementation include: nephrolithiasis and increased incidence of cardiovascular events.
Therapies for PO act by reducing bone resorption, stimulating bone formation (anabolic therapy) or both.
All pharmacologic approaches can reduce vertebral fracture risk, and some measures reduce the non-vertebral and hip fractures.
Initial treatment with anabolic agents is recommended in women at very high risk unless contraindicated.
Most guidelines recommend bisphosophonates as initial treatment for women with PO, given their efficacy, safety and convenience, and enduring effects after discontinuation.
Oral and intravenous bisphosophonates approved for postmenopausal osteoporosis reduce the risk of vertebral fracture.
All bisphosophonates, but ibandronate reduce the risk of hip and non-vertebral fractures.
Oral bisphosophonates are poorly absorbed, and can cause UGI mucosal irritation.
Intravenous zolendronateis preferred in patients who have GI side effects, and those with the esophageal dysfunction.
10 years after trial initiation, zoledronate administered at baseline and at five years was effective in preventing vertebral fractures in early postmenopausal women (Bolland MJ).
Long-term use of bisphosphonates has been associated with jaw necrosis and atypical femur fractures: the estimated risk of osteonecrosis of the jaw and atypical femur fractures are very low with the doses used for PO.
Denosumab lowers the risk of spine, hip and non-vertebral fractures compared with placebo.
Gains in bone mineral density are greater with denosumab than bisphosphonates, and is rarely associated with jaw necrosis, atypical femur fracture or hypocalcemia.
Concerns exist about accelerated bone resorption and rapid bone loss after discontinuation of denosumab therapy.
Parathyroid hormone receptor agonist include teriparatide and abaloparatide.
Treatment with these agents reduces vertebral, and non-vertebral fracture risk over 18 to 24 months: need a drug reduces the incidence of hip fractures.
These agents require daily injections.
Anti-resorptive therapy is indicated after PTH receptor agonist therapy is complete and such therapy increases bone mineral density further.
PTH, receptor agonist still have limited safety and efficacy data and should be avoided impatience with increased risk for osteosarcoma – Paget’s disease of the bone or skeletal irradiation.
Romosozumab is a monthly subcutaneous injection approved for postmenopausal osteoporosis.
Decreases both vertebral, and non-vertebral fractures.
Following Romosozumab’s use it should be followed by treatment with bisphophonates or denosumab.
It has a black box warning for cardiovascular events, and should be the initial therapy in postmenopausal women with very high risk for fracture.
Patients with pot menopausal osteoporosis should be monitored for treatment results.
The presence of decreasing bone mineral density or the occurrence of multiple fractures should prompt reconsideration for alternative therapy.
The duration of bisphosophonate therapy is unclear, but most recommend a break after five years to lower the risk of atypical hip fractures.
