 Percutaneous Coronary Intervention (PCI), also known as coronary angioplasty or stenting, is a common medical procedure used to treat coronary artery disease.
Percutaneous Coronary Intervention (PCI), also known as coronary angioplasty or stenting, is a common medical procedure used to treat coronary artery disease.
Percutaneous coronary intervention (PCI) is a non-surgical procedure used to treat narrowing of the coronary arteries of the heart found in coronary artery disease.
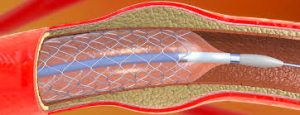
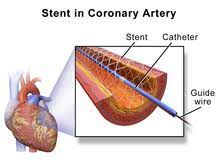
It involves the placement of a thin catheter, into a blocked or narrowed coronary artery to restore blood flow to the heart muscle.
It involves coronary artery with stenting, which is the insertion of a permanent wire-meshed tube that is either drug eluting (DES) or composed of bare metal (BMS).
During a PCI procedure, a small balloon at the tip of the catheter is inflated to widen the blocked or narrowed artery, allowing for improved blood flow.
Percutaneous coronary intervention (PCI) is a non-surgical procedure used to treat narrowing of the coronary arteries of the heart found in coronary artery disease.
A stent delivery balloon from the angioplasty catheter is inflated to force contact between the struts of the stent and the vessel wall widening the blood vessel diameter.
After accessing the blood stream through the femoral or radial artery, the procedure uses coronary catheterization to visualize the blood vessels on X-ray imaging.
A coronary angioplasty, using a balloon catheter in which a deflated balloon is advanced into the obstructed artery and inflated to relieve the narrowing; stents can be deployed to keep the blood vessel open.
Primary PCI is the emergent use of PCI in people with acute myocardial infarction, especially where there is evidence of heart damage on the electrocardiogram.
It is also used in people after other forms of myocardial infarction or unstable angina where there is a high risk of further events.
It may be used in people with stable angina pectoris, particularly if the symptoms are difficult to control with medication.
PCI is an alternative to coronary artery bypass grafting (CABG).
PCI is most commonly guided by angiography, although it is unable to provide information about plaque morphology, vascular remodeling, and the burden of atherosclerosis in the vessel.
Angiography with PCI has limited ability to identify underexpansion of implanted stents, malapposition of the stent to the vessel, wall, and dissections in the vessels from PCI.
Intravascular ultrasound guided PCI reduces incidence of cardiovascular events, including death from cardiac causes and stent thrombosis, but it is infrequently use because of diffult image interpretation.
Imaging guided PCI is associated with better clinical outcomes, than angiography guided PCI.
Optical coherence tomography, guided PCI among patients with complex coronary artery bifurcation lesions results in lower incidence of major adverse cardiac events than angiography guided PCI.
Percutaneous coronary angioplasty is one of the most common procedures performed during U.S. hospital stays.
It involves combining coronary angioplasty with stenting with insertion of a permanent wire-meshed tube that is either drug eluting (DES) or composed of bare metal (BMS).
The stent delivery balloon is inflated to force contact between the struts of the stent and the vessel wall, with then widening the blood vessel diameter.
PCI is used primarily to open a blocked coronary artery and restore arterial blood flow to heart tissue, without requiring open-heart surgery.
PCI usually includes the insertion of stents, bare-metal stents, or drug-eluting stents, and fully resorbable vascular scaffolds.
Resorbable vascular scaffolds are naturally dissolving stents.
The use of stents has been shown to be important during the first three months after PCI; after that, the artery can remain open on its own.
PCI use depends on many factors and may be appropriate for patients with stable coronary artery disease if they meet certain criteria, such as having any coronary stenosis greater than 50 percent or having angina symptoms that are unresponsive to medical therapy.
Although PCI may not provide any greater help in preventing death or myocardial infarction over oral medications for patients with stable coronary artery disease, it likely provides better relief of angina.
Coronary angioplasty uses a balloon catheter in which a deflated balloon is advanced into the obstructed artery and inflated to relieve the narrowing; certain devices such as stents can be deployed to keep the blood vessel open.
Primary PCI refers to the emergent use of PCI in people with acute heart attack, especially where there is evidence of heart damage on the electrocardiogram.
PCI is also used in people after other forms of myocardial infarction or unstable angina where there is a high risk of further events.
Finally, PCI may be used in people with stable angina pectoris, particularly if the symptoms are difficult to control with medication. Among patients with stable angina, who were receiving little or no antianginal medication and had objective evidence of ischemia, PCI resulted in lower angina symptoms score than a placebo procedure, indicating a better health status with respect to angina (ORBITA-2 investigators).
PCI is an alternative to coronary artery bypass grafting.
The the procedure uses coronary catheterization to visualize the blood vessels on X-ray imaging, via the femoral or radial artery access.
In some cases, a small metal mesh tube stent is inserted into the artery to keep it open after the balloon is deflated and removed.
The stent acts as a scaffold, providing structural support and preventing the artery from re-narrowing.
PCI is typically performed in a specialized cardiac catheterization laboratory by an interventional cardiologist.
It is a minimally invasive procedure compared to open-heart surgery and typically requires a shorter hospital stay and recovery period.
PCI is commonly used to relieve symptoms of chest pain improve quality of life, and reduce the risk of heart attack in patients with significant coronary artery disease.
Early reperfusion of a culprit vessel with primary percutaneous coronary intervention in patients with ST segment elevation, myocardial infarction, and an early invasive strategy in patients with non-STEMI improves cardiovascular outcomes, regardless of chronological age.
In patients with multivessel coronary artery disease, randomized trials have shown that additional PCI of non-culprit lesions with the goal of complete revascularization is not superior to PCI of only the culprit lesion.
Among patients with STEMI, or high-risk, NSTEMI multivessel coronary artery disease, fractional flow reserve (FFR) guided revascularization did not show a lower risk of composite death from any cause, myocardial infarction, or unplanned revascularization, than culprit lesion only PCI at 4.8 years (FULL REVASC Trial investigators).
Complete revascularization shows evidence for improved reduction in the risk of cardiovascular death or new myocardial infarction and improvements in quality of life.
With as extensive blockages, background of diabetes, CABG may be superior.
PCI is used primarily to open a blocked coronary artery and restore arterial blood flow to heart tissue, without requiring open-heart surgery.
PCI usually includes the insertion of stents, such as bare-metal stents, drug-eluting stents, and fully resorbable vascular scaffolds, or naturally dissolving stents.
The use of stents has been shown to be important during the first three months after PCI; after that, the artery can remain open on its own.
In patients with acute coronary syndromes, PCI may be appropriate.
In patients with severe blockages, such as ST-segment elevation myocardial infarction (STEMI), PCI can be critical to survival as it reduces deaths, myocardial infarctions and angina compared with medication.
For patients with either non-ST-segment elevation myocardial infarction (nSTEMI) or unstable angina, treatment with medication and/or PCI depends on a patient’s risk assessment.
The door-to-balloon time is used as a quality measure for hospitals to determine the timeliness of primary PCI.
The use of PCI plus angina medications in stable angina patients may reduce the number of patients with angina attacks for up to 3 years following the therapy, but does not reduce the risk of death, future myocardial infarction or need for other interventions.
Coronary angioplasty has a number of risks, but major procedural complications are uncommon.
The patient is usually awake during angioplasty, in order to monitor the patient’s symptoms.
Bleeding from the insertion points in the groin or wrist is common, in part due to the use of antiplatelet drugs.
Bruising is expected with PCI, and occasionally a hematoma may form.
The flow from the artery into a hematoma may cause a pseudoaneurysm, which may require surgical repair.
Infection at the skin puncture site is rare and dissection of the access blood vessel is uncommon.
Deterioration of kidney function can occur in patients with pre-existing kidney disease, but kidney failure requiring dialysis is rare.
Vascular access complications are less common and less serious when the procedure is performed via the radial artery.
The most serious risks are PCI are death, stroke, ventricular fibrillation, ventricular tachycardia, myocardial infarction and aortic dissection.
A heart attack during or shortly after the PCI procedure occurs in 0.3% of cases; this may require emergency coronary artery bypass surgery.
Heart muscle injury as indicated by elevated levels of CK-MB, troponin I, and troponin T may occur in up to 30% of all PCI procedures.
Such elevation of enzymes is associated with later clinical outcomes such as higher risk of death, subsequent MI, and need for repeat revascularization procedures.
Angioplasty carried out shortly after an MI has a risk of causing a stroke, but this is less than the risk of a stroke following thrombolytic drug therapy.
The mortality rate during angioplasty is 1.2%.
The risk of complications from PCI is higher in:
People aged 65 and older
People who have kidney disease or diabetes
Women
People who have poor pumping function in their hearts
People who have extensive heart disease and blockages
Balloon angioplasty: the inflation of a balloon within the coronary artery to crush the plaque into the walls of the artery.
Balloon angioplasty is still done as a part of nearly all percutaneous coronary interventions, but it is rarely the only procedure performed:
Implantation of stents
Debulking strategies
Rotational atherectomy
Orbital atherectomy
Laser atherectomy
Brachytherapy
Coronary intravascular lithotripsy (IVL)
The angioplasty procedure usually consists of most of the following steps:
The femoral artery in the leg or the radial artery in the arm is punctured with a needle and a small wire is passed into the artery.
Once access into the artery is established a sheath introducer is placed over the wire into the artery to allow catheters to be advanced into the artery and to control bleeding.
Through this sheath, a long, flexible, soft plastic tube guiding catheter is pushed.
The tip of the guiding catheter is placed at the mouth of the coronary artery, and allows for radio-opaque dyes to be injected into the coronary artery, so that the disease state and location can be readily assessed.
The cardiologist estimates the size of the coronary artery and selects the type of balloon catheter and coronary guidewire that will be used during the intervention.
Heparin is given to maintain blood flow.
The cardiologist guides the wire through the coronary artery to the site of the stenosis or blockage, where the tip of the wire is then passed across the blockage.
The tip of the angioplasty or balloon catheter is hollow and is then inserted at the back of the guidewire; the guidewire is now inside of the angioplasty catheter.
The angioplasty catheter is gently pushed forward, until the deflated balloon is inside of the blockage.
The balloon is then inflated, and it compresses the atheromatous plaque and stretches the artery wall to expand.
If a stent was on the balloon, then it will be implanted to support the new stretched open position of the artery from the inside.
Traditional bare-metal stents (BMS) provide a mechanical framework that holds the artery wall open, preventing stenosis, or narrowing, of coronary arteries.
Newer drug-eluting stents (DES) are traditional stents with a polymer coating containing drugs that prevent cell proliferation.
These antiproliferative drugs are released slowly over time to help prevent tissue growth that can block the artery.
These types of stents help prevent restenosis of the artery through physiological mechanisms that rely upon the suppression of tissue growth at the stent site and local modulation of the body’s inflammatory and immune responses.
Most current FDA-approved drug-eluting stents use sirolimus (also known as rapamycin), everolimus and zotarolimus.
Late stent thrombosis occurs in 0.9% of patients and is fatal in about one-third of cases when the thrombosis occurs.
Increased attention to antiplatelet medication duration and new generation stents, such as everolimus-eluting stents, have dramatically reduced concerns about late stent thrombosis.
After placement of a stent or scaffold, the patient takes two antiplatelet medications for several months to help prevent blood clots.
In primary PCI, angiography may demonstrate thrombus inside the coronary arteries.
There is no evidence that routine clot aspiration improves outcomes.
Lesions with a high degree of calcium deposition within the vessel wall, especially if the calcium is circumferential, are considered to be hard to dilate in regards to balloon angioplasty.
Complex lesions predict poor outcome in percutaneous coronary intervention (PCI).
Calcium lesion modification is needed before implantations of stents, by creating cracks in the calcium within the vessel wall in order to increase the likelihood of successful expansion of the stenosis and delivery of the final stent.
Traditionally this achieved by balloon angioplasty or debulking strategies including rotational, orbital and laser atherectomy.
Most studies have found that CABG offers advantages in reducing death and myocardial infarction in people with multivessel blockages compared with PCI.
Current concepts recognize that after three months the artery has adapted and healed and no longer needs the stent.
Complete revasculariztion of all stenosed coronary arteries after a STEMI is more efficacious in terms of major adverse cardiac events and all-cause mortality, while being safer than culprit-vessel-only approach.
The studies comparing stenting as used in PCI to medical therapy alone in symptomatic stable coronary artery disease:
This showed there was no mortality advantage to stenting in stable CAD, though there was earlier relief of symptoms which equalized by five years.
The ISCHEMIA trial has confirmed that invasive procedures (PCI or CABG) do not reduce death or heart attacks compared to medical therapy alone for stable angina.
Patients with angina experienced improved quality of life with PCI compared to medical therapy.
PCI may be appropriate for patients with stable coronary artery disease if they have any coronary stenosis greater than 50 percent or having angina symptoms that are unresponsive to medical therapy.
PCI may not provide any greater help in preventing death or myocardial infarction over oral medication for patients with stable coronary artery disease, it likely provides better relief of angina.
With acute coronary syndromes, PCI may be appropriate.
In patients with severe blockages, such as ST-segment elevation myocardial infarction (STEMI), PCI reduces deaths, myocardial infarctions and angina compared with medication.
For patients with either non-ST-segment elevation myocardial infarction (nSTEMI) or unstable angina, treatment with medication and/or PCI depends on a patient’s risk assessment.
The use of PCI in addition to anti-angina medication in stable angina may reduce the number of patients with angina attacks for up to 3 years following the therapy,[9] but does not reduce the risk of death, future myocardial infarction or need for other interventions.
Coronary angioplasty is usually performed using invasive catheter-based procedures by an interventional cardiologist.
The patient is usually awake during angioplasty.
If symptoms indicate the procedure is causing ischemia the cardiologist may alter or abort part of the procedure.
Bleeding from the insertion at the femoral artery or radial artery is common, in part due to the use of antiplatelet drugs.
Occasionally a hematoma may form.
Flow from the artery into the hematoma may continue as a pseudoaneurysm which requires surgical repair.
Infection at the skin puncture site is rare and dissection of the access blood vessel is uncommon.
Deterioration of kidney function can occur in patients with pre-existing kidney disease, but kidney failure requiring dialysis is rare.
Vascular access complications are less common and less serious when the procedure is performed via the radial artery.
Utilizing the radial or wrist artery instead of the artery in the volume minimizes bleeding and complications.
A heart attack during or shortly after the procedure occurs in 0.3% of cases.
Heart muscle injury characterized by elevated levels of CK-MB, troponin I, and troponin T may occur in up to 30% of all PCI procedures.
Elevated enzymes have been associated with later clinical outcomes such as higher risk of death, subsequent MI, and need for repeat revascularization procedures.
Angioplasty carried out shortly after an MI has a risk of causing a stroke, but this is less than the risk of a stroke following thrombolytic drug therapy.
The mortality rate during angioplasty is 1.2%.
Sometimes chest pain can occur during angioplasty as the balloon briefly blocks off the blood supply to the heart.
This complications is higher in:
People aged 65 and older
People who have kidney disease or diabetes
Women
People who have poor pumping function in their hearts
People who have extensive heart disease and blockages
Balloon angioplasty is commonly used to describe the inflation of a balloon within the coronary artery to crush the plaque into the walls of the artery.
While balloon angioplasty is still done as a part of nearly all percutaneous coronary interventions, it is rarely the only procedure performed:
Implantation of stents
Debulking strategies
Rotational atherectomy
Orbital atherectomy
Laser atherectomy
Brachytherapy
Coronary intravascular lithotripsy (IVL)
The femoral artery in the leg or the radial artery in the arm is punctured with a needle and a small wire is passed into the artery.
Once access into the artery is gained, a sheath introducer is placed over the wire into the artery to allow catheters to be advanced into the artery and to control bleeding.
Through this sheath, a long, flexible, soft plastic tube called a guiding catheter is pushed.
The tip of the guiding catheter is placed at the coronary artery.
The guiding catheter allows for radio-opaque dyes to be injected into the coronary artery, so that the disease state and location can be readily assessed using real time X-ray visualization.
With X-ray visualization, the cardiologist can estimate the size of the coronary artery and selects the type of balloon catheter and coronary guidewire that will be used during the case.
Heparin is used to prevent the formation of clots) is given to maintain blood flow.
The coronary guidewire, which is an extremely thin wire with a radio-opaque flexible tip, is inserted through the guiding catheter and into the coronary artery to the site of the stenosis or blockage.
The tip of the wire is then passed across the blockage.
When the guidewire is inside of the angioplasty catheter, the angioplasty catheter is pushed forward, until the deflated balloon is inside of the blockage.
The balloon is then inflated, and it compresses the atheromatous plaque and stretches the artery wall to expand.
If a stent was on the balloon, then it will be implanted to support the new stretched open position of the artery from the inside.
Traditional bare-metal stents (BMS) provide a mechanical framework that holds the artery wall open, preventing stenosis, or narrowing, of coronary arteries.
Newer drug-eluting stents (DES) are traditional stents with a polymer coating containing drugs that prevent cell proliferation.
The antiproliferative drugs are released slowly over time, helping prevent tissue growth that can block the artery.
These types of stents prevent restenosis of the artery through suppression of tissue growth at the stent site and local modulation of the body’s inflammatory and immune responses.
Drug-eluting stents include paclitaxel-eluting stent and the sirolimus-eluting stent, everolimus, zotarolimus and Biolimus A9-eluting stents.
Late stent thrombosis occurs in 0.9% of patients and is fatal in about one-third of cases when the thrombosis occurs.
Increased use antiplatelet medication duration and new generation stents have reduced concerns about late stent thrombosis.
After placement of a stent or scaffold, the patient needs dual antiplatelet medications for several months to help prevent blood clots.
Antiplatelet drugs ticagrelor and prasurgrel act more quickly in patients than clopidogrel and is recommended may be used over clopidogrel after PCI.
The length of time a patient needs to be on dual antiplatelet therapy is individualized based risks of ischemic events and bleeding risk.
In primary PCI, angiography may demonstrate thrombus inside the coronary arteries, but there is no evidence that routine clot aspiration improves outcomes.
Arteries with a high degree of calcium deposition within the vessel wall, especially if the calcium is circumferential, are considered to be hard to dilate in regards to balloon angioplasty.
Calcium lesion modification is needed before implantations of stents: by creating cracks in the calcium within the vessel wall to increase the likelihood of successful expansion of the stenosis and delivery of the final stent.
Calcium lesion modification is traditionally achieved by balloon angioplasty or debulking strategies including rotational, orbital and laser atherectomy.
Most studies have found that CABG offers advantages in reducing death and myocardial infarction in people with multivessel blockages compared with PCI.
Among patients with hemodynamically stable condition with STEMI, and multivessel coronary artery disease, immediate multivessel PCI was non-inferior to staged multivessel PCI with respect to the risk of death from any cause, non-fatal, myocardial infarction, stroke, unexplained, ischemia driven revascularization, or hospitalization for heart failure at one year(MULTISTA,RSAMI investigators).
After three months the coronary artery has adapted and healed and no longer needs the stent.
Complete revasculariztion of all stenosed coronary arteries after a STEMI is more efficacious in terms of major adverse cardiac events and all-cause mortality, while being safer than culprit-vessel-only approach.
The COURAGE study compared stenting as used in PCI to medical therapy alone in symptomatic stable coronary artery disease (CAD), and it showed there was no mortality advantage to stenting in stable CAD, though there was earlier relief of symptoms which equalized by five years.
The ORBITA study found that following percutaneous coronary intervention there was no statistically significant difference in exercise time compared with medical therapy.
In a randomized, double blind, placebo controlled trial, PCI was shown as an effective antianginal treatment in patients with stable angina, who had objective evidence of ischemia (ORBITA-2).
The ISCHEMIA trial confirmed that invasive procedures (PCI or CABG) did not reduce death or heart attacks compared to medical therapy alone for stable angina.
Patients with angina experienced improved quality of life with PCI compared to medical therapy.
Among patient 75 years of age or older with myocardial infarction and multi vessel disease, those who underwent complete revascularization based on physiologically guided therapy, had a lower risk of death, myocardial infarction, stroke, or ischemia-driven revascularization at one year, than those who received culprit lesion only PCI (FIRE trial investigators).
In the COMPLETE trial of complete versus culprit only revascularization strategies to treat multivessel disease after early PCI for STEMI showed a 26% lower risk of death from cardiovascular causes or myocardial infarction, and a greater improvement in angina scores after three years of follow up among patients who have been assigned to undergo complete revascularization of angiographically significant non-culprit lesions, than among patients who had no further revascularization.
Among patients with coronary disease who are undergoing trans catheter aortic valve implantation, PCI was associated with the lower risk of composite of death from any cause, myocardial infarction, or urgent revascularization at a median follow up of two years, than conservative treatment.
